Hypertrophy Of The Right Ventricle Is A Compensatory Response To
Breaking News Today
Mar 26, 2025 · 6 min read
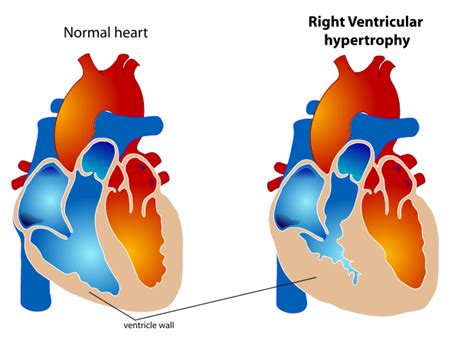
Table of Contents
Hypertrophy of the Right Ventricle: A Compensatory Response to Pulmonary Hypertension and Other Conditions
Right ventricular hypertrophy (RVH) is a significant cardiac adaptation, often representing the heart's attempt to compensate for increased workload. While it initially improves cardiac output, prolonged RVH can lead to right heart failure and ultimately, death. Understanding the underlying causes and the mechanisms involved is crucial for effective diagnosis and management. This comprehensive article delves into the various conditions that trigger RVH, focusing primarily on its role as a compensatory response to pulmonary hypertension. We will also explore other contributing factors and the implications for patient health.
Pulmonary Hypertension: The Primary Driver of RVH
Pulmonary hypertension (PH), characterized by elevated blood pressure in the pulmonary arteries, is the most common cause of RVH. The increased pressure necessitates greater force from the right ventricle to pump blood into the lungs. This sustained increase in afterload forces the right ventricle to work harder, leading to its thickening and enlargement – hypertrophy.
Mechanisms of RVH in Pulmonary Hypertension
Several mechanisms contribute to RVH in the context of PH:
-
Increased wall stress: The elevated pulmonary arterial pressure directly increases the wall stress on the right ventricle. The heart muscle responds by thickening to maintain adequate contractility. This is a classic example of the Frank-Starling mechanism at play, albeit in a pathological context.
-
Neurohormonal activation: PH triggers the activation of the renin-angiotensin-aldosterone system (RAAS) and the sympathetic nervous system. These systems contribute to increased vasoconstriction, fluid retention, and cardiac remodeling, further exacerbating RVH.
-
Genetic predisposition: Certain genetic factors might predispose individuals to developing RVH in response to PH. These genetic influences can impact the heart's response to stress and its ability to adapt effectively.
-
Inflammatory processes: Inflammation plays a significant role in the pathogenesis of PH. Inflammatory mediators can directly damage the right ventricular myocardium, further contributing to RVH and eventual dysfunction.
Types of Pulmonary Hypertension and RVH
Different types of pulmonary hypertension (classified by the World Health Organization) are associated with varying degrees and patterns of RVH:
-
Group 1 PH (PAH): This group includes idiopathic PAH, heritable PAH, and PAH associated with connective tissue diseases, HIV infection, and drug use. RVH is a prominent feature in these conditions, often progressing rapidly if left untreated.
-
Group 2 PH (PH due to left heart disease): Left-sided heart failure leads to increased pulmonary venous pressure, which in turn raises pulmonary arterial pressure, causing RVH. This type of RVH is often a secondary consequence of a more significant underlying cardiac problem.
-
Group 3 PH (PH due to lung diseases and/or hypoxia): Chronic obstructive pulmonary disease (COPD), interstitial lung disease, and sleep apnea can cause PH and subsequent RVH. Hypoxia, or low oxygen levels in the blood, also contributes to vascular remodeling and PH.
-
Group 4 PH (PH due to chronic thromboembolic disease): Recurrent pulmonary emboli can obstruct pulmonary arteries, leading to increased pressure and RVH. This is a potentially life-threatening condition requiring prompt intervention.
-
Group 5 PH (PH with unclear and/or multifactorial mechanisms): This group encompasses various conditions, including hematological disorders, systemic disorders, and others that contribute to PH and RVH.
Other Causes of Right Ventricular Hypertrophy
While PH is the most significant cause, several other conditions can lead to RVH:
-
Congenital heart defects: Conditions like tetralogy of Fallot and tricuspid atresia place significant strain on the right ventricle, resulting in hypertrophy.
-
Valvular heart disease: Pulmonary stenosis, tricuspid regurgitation, and other valvular diseases can increase the right ventricular workload and cause hypertrophy.
-
Pulmonary embolism: A single, large pulmonary embolism can acutely overload the right ventricle, although this often presents as right ventricular dysfunction rather than sustained hypertrophy.
-
Cardiac tumors: Tumors obstructing blood flow can cause RVH.
-
Chronic lung diseases: Conditions such as cystic fibrosis, which lead to increased pulmonary vascular resistance, can eventually cause RVH.
Consequences of Right Ventricular Hypertrophy
While initially compensatory, sustained RVH is detrimental to cardiac function. The thickened right ventricle becomes less efficient, ultimately leading to:
-
Right heart failure: The right ventricle's inability to effectively pump blood leads to fluid buildup in the body, causing peripheral edema, ascites, and jugular venous distention.
-
Decreased cardiac output: The hypertrophied but inefficient right ventricle reduces the overall blood flow to the lungs, impacting oxygenation.
-
Arrhythmias: RVH can lead to various arrhythmias, including atrial fibrillation and ventricular tachycardia, increasing the risk of sudden cardiac death.
-
Sudden cardiac death: In severe cases, the weakened and dysfunctional right ventricle can fail, resulting in sudden death.
Diagnosis of Right Ventricular Hypertrophy
Diagnosing RVH involves a combination of techniques:
-
Echocardiography: This is the primary diagnostic tool. Echocardiography measures the right ventricular dimensions, wall thickness, and function, allowing for the assessment of hypertrophy.
-
Electrocardiography (ECG): ECG can show characteristic changes associated with RVH, such as right axis deviation and tall R waves in the right precordial leads. However, ECG findings can be subtle and may not always accurately reflect the severity of RVH.
-
Cardiac MRI: Provides more detailed images of the right ventricle, allowing for precise assessment of its size, mass, and function.
-
Cardiac catheterization: This invasive procedure directly measures pulmonary artery pressure and right ventricular pressure, providing crucial information about the severity of PH and the extent of RVH.
Treatment of Right Ventricular Hypertrophy
Treatment strategies for RVH focus on addressing the underlying cause and managing symptoms. Treatment modalities vary depending on the etiology:
-
Treatment of PH: Specific treatments for PH include medications that target vasoconstriction, such as endothelin receptor antagonists, phosphodiesterase-5 inhibitors, and prostacyclin analogs.
-
Treatment of valvular disease: Valvular replacement or repair may be necessary if valvular dysfunction is contributing to RVH.
-
Management of heart failure: Diuretics, ACE inhibitors, and other medications are used to manage symptoms of right heart failure.
-
Lifestyle modifications: Dietary changes, regular exercise (when appropriate), and smoking cessation can improve overall cardiovascular health and slow the progression of RVH.
-
Surgical interventions: In some cases, surgery may be necessary to address underlying structural abnormalities or to improve right ventricular function.
Conclusion: A Complex Adaptive Response
Right ventricular hypertrophy is a complex adaptive response, primarily triggered by pulmonary hypertension but also by other conditions leading to increased right ventricular workload. While initially beneficial, sustained RVH ultimately compromises cardiac function, leading to potentially life-threatening complications. Early diagnosis, targeted treatment of the underlying cause, and careful management of symptoms are crucial for improving patient outcomes and preventing the progression of this serious condition. The prognosis for individuals with RVH varies considerably depending on the underlying etiology, the severity of hypertrophy, and the effectiveness of treatment. Continuous monitoring and proactive management are essential for maximizing the chances of a favorable outcome. Further research continues to explore novel therapeutic approaches to mitigate the adverse effects of RVH and improve the quality of life for those affected.
Latest Posts
Latest Posts
-
Nos Alojamos En Un Hotel Malo De La Capital
Mar 29, 2025
-
From A Security Perspective The Best Rooms Are
Mar 29, 2025
-
Which Of The Following Is True Of Psychologically Healthy People
Mar 29, 2025
-
The Ultimate Goal Of Lean Operations Is To Have
Mar 29, 2025
-
La Esposa De Mi Padre Pero No Soy Su Hijo
Mar 29, 2025
Related Post
Thank you for visiting our website which covers about Hypertrophy Of The Right Ventricle Is A Compensatory Response To . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
