Lack Of Α-antitrypsin In Emphysema Causes Quizlet
Breaking News Today
Mar 24, 2025 · 6 min read
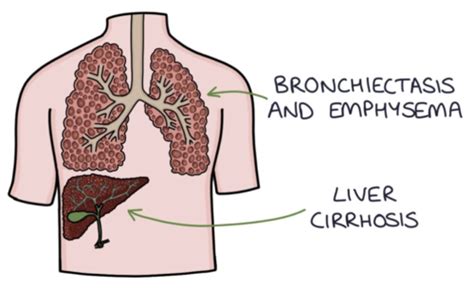
Table of Contents
The Crucial Role of Alpha-1 Antitrypsin Deficiency in Emphysema: A Comprehensive Guide
Emphysema, a debilitating lung disease characterized by the destruction of alveoli (tiny air sacs in the lungs), significantly impacts breathing and overall quality of life. While smoking is a leading risk factor, a significant percentage of emphysema cases stem from a genetic deficiency: a lack of alpha-1 antitrypsin (AAT). This article delves deep into the connection between AAT deficiency and emphysema, exploring its causes, mechanisms, symptoms, diagnosis, and management. We will move beyond a simple quizlet-style overview to provide a comprehensive understanding of this complex interplay.
Understanding Alpha-1 Antitrypsin (AAT)
Alpha-1 antitrypsin is a serine protease inhibitor (serpin), primarily produced by the liver. Its crucial function lies in protecting the lungs from the damaging effects of neutrophil elastase, a potent enzyme released by neutrophils, a type of white blood cell involved in fighting infection. Neutrophil elastase, while vital in combating pathogens, can also break down the delicate elastin fibers that provide structural support to the alveoli. AAT acts as a crucial shield, neutralizing the elastase and preventing excessive lung tissue damage.
The Genetic Basis of AAT Deficiency
AAT deficiency is inherited in an autosomal codominant pattern. This means that an individual needs only one copy of a mutated gene to experience reduced AAT levels. The most common mutation is known as the Z allele. Individuals with two copies of the Z allele (ZZ genotype) have the most severe AAT deficiency, while those with one copy of the Z allele (MZ genotype) usually have milder forms. Other less common mutations also contribute to AAT deficiency.
How AAT Deficiency Leads to Emphysema
In individuals with AAT deficiency, insufficient levels of AAT fail to adequately neutralize neutrophil elastase. This unchecked elastase activity leads to the progressive destruction of alveolar walls, resulting in emphysema. The process is often gradual, with symptoms initially appearing in mid-adulthood or later. The severity of emphysema directly correlates with the degree of AAT deficiency; individuals with the ZZ genotype tend to experience more severe and early-onset disease.
Clinical Manifestations of Emphysema in AAT Deficiency
Emphysema related to AAT deficiency presents similarly to other forms of emphysema, but with some notable distinctions:
Respiratory Symptoms:
- Shortness of breath (dyspnea): This is often the earliest and most prominent symptom, initially appearing during exertion but progressing to rest.
- Chronic cough: A dry or productive cough is common, often worsening with activity or exposure to irritants.
- Wheezing: While not always present, wheezing can indicate airway obstruction.
- Chest tightness: A feeling of constriction or pressure in the chest.
- Increased sputum production: Individuals may produce more mucus than usual, sometimes with blood.
Systemic Manifestations:
AAT deficiency can impact organs beyond the lungs. This is due to the widespread presence and function of AAT. Some individuals may experience:
- Liver disease: Accumulation of misfolded AAT in the liver can lead to cirrhosis or liver cancer. This is more likely in individuals with the ZZ genotype.
- Skin manifestations: Some individuals report increased skin dryness or bruising.
- Vasculitis: Inflammation of blood vessels can occur in rare cases.
Diagnosing AAT Deficiency and Emphysema
Diagnosing AAT deficiency and related emphysema requires a multifaceted approach:
1. Medical History and Physical Examination:
A detailed medical history, including family history of respiratory disease or liver problems, is crucial. A physical exam may reveal decreased breath sounds, wheezing, and increased respiratory effort.
2. Spirometry:
This pulmonary function test measures lung capacity and airflow. Spirometry often reveals decreased forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC), consistent with obstructive lung disease.
3. Alpha-1 Antitrypsin Blood Test:
This is the definitive test for AAT deficiency. It measures the concentration of AAT in the blood. Low levels confirm deficiency, and further genetic testing may be needed to determine the specific genotype (e.g., ZZ, MZ).
4. Imaging Studies:
Chest X-rays and CT scans can visualize the extent of lung damage. Emphysema is characterized by hyperinflation (increased air trapping) and loss of lung volume.
5. Genetic Testing:
This helps determine the specific AAT genotype, allowing for a more precise assessment of disease severity and prognosis.
Management and Treatment of Emphysema in AAT Deficiency
The management of emphysema in AAT deficient individuals aims to alleviate symptoms, slow disease progression, and improve quality of life. This involves a combination of:
1. Smoking Cessation:
This is the single most important intervention for all forms of emphysema, significantly slowing disease progression. Support groups and cessation programs are invaluable.
2. Bronchodilators:
These medications, including inhaled beta-agonists and anticholinergics, help relax airway muscles and improve airflow.
3. Inhaled Corticosteroids:
While not as effective as in asthma, some patients may benefit from inhaled corticosteroids to reduce airway inflammation.
4. Oxygen Therapy:
Supplemental oxygen is essential for individuals with severe hypoxemia (low blood oxygen levels). This can significantly improve exercise tolerance and overall well-being.
5. Pulmonary Rehabilitation:
A comprehensive program including exercise training, education, and psychosocial support can enhance exercise capacity, reduce dyspnea, and improve quality of life.
6. Augmentation Therapy:
For individuals with severe AAT deficiency, augmentation therapy involves regular intravenous infusions of purified AAT. This therapy aims to supplement deficient AAT levels and potentially slow disease progression. The effectiveness of augmentation therapy is still under investigation, with ongoing research exploring optimal dosing and long-term effects.
7. Lung Volume Reduction Surgery (LVRS):
In selected cases of severe emphysema, LVRS may be considered to remove damaged lung tissue, improving lung function. This is a complex procedure with potential risks and is not suitable for all individuals.
8. Lung Transplant:
For individuals with end-stage lung disease, a lung transplant may be a life-saving option. This is a major surgical procedure with significant risks and requires lifelong immunosuppression.
Living with Emphysema and AAT Deficiency: Prognosis and Support
The prognosis for emphysema in AAT deficiency varies depending on the severity of the deficiency, the presence of other risk factors (like smoking), and the individual's response to treatment. Early diagnosis and aggressive management are crucial in slowing disease progression and improving quality of life.
Support groups and patient advocacy organizations play a vital role in providing emotional, educational, and practical support for individuals living with AAT deficiency and emphysema. These organizations can connect individuals with healthcare professionals, resources, and other affected individuals, fostering a sense of community and shared experience.
Conclusion: A Holistic Perspective
AAT deficiency is a significant contributor to emphysema, highlighting the complex interplay between genetic predisposition and environmental factors. Understanding the crucial role of AAT in lung protection, the mechanisms of disease pathogenesis, and the available treatment options is essential for effective disease management. A holistic approach, integrating medical interventions, lifestyle modifications (especially smoking cessation), and psychosocial support, is vital in optimizing the quality of life for individuals affected by this debilitating condition. Ongoing research continues to unveil new insights into the intricacies of AAT deficiency and emphysema, paving the way for improved diagnostic tools and therapeutic strategies. Early detection, proactive management, and access to supportive resources are critical for individuals living with AAT deficiency-related emphysema to live full and productive lives.
Latest Posts
Latest Posts
-
Examen De Manejo Nj Preguntas Y Respuestas
Mar 26, 2025
-
Which Of The Following Statements About Trophic Cascades Is True
Mar 26, 2025
-
Las Ramblas Es Un Bulevar Muy Famoso En Madrid
Mar 26, 2025
-
What Is The Purpose Of Improving Your Business Writing
Mar 26, 2025
-
Tina Jones Respiratory Shadow Health Objective Data
Mar 26, 2025
Related Post
Thank you for visiting our website which covers about Lack Of Α-antitrypsin In Emphysema Causes Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
