One Difference Between Osteoarthritis And Rheumatoid Arthritis Is That Quizlet
Breaking News Today
Mar 23, 2025 · 6 min read
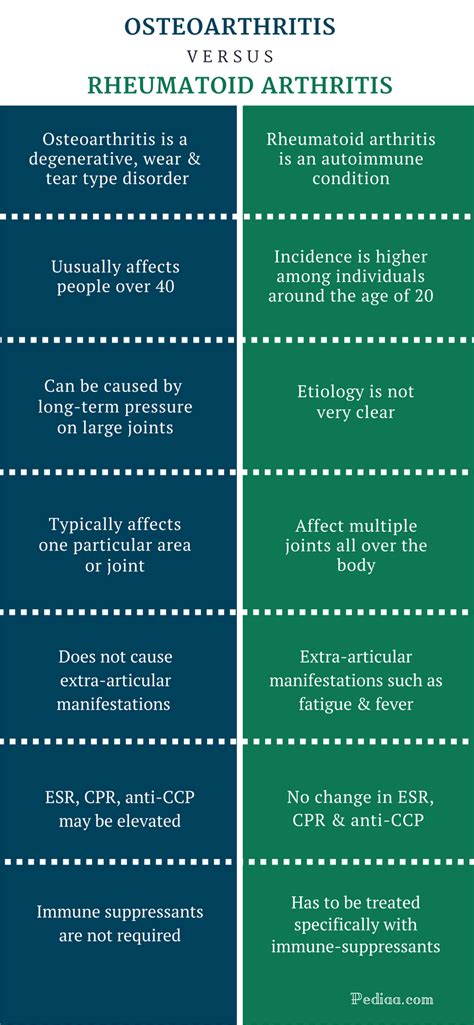
Table of Contents
One Difference Between Osteoarthritis and Rheumatoid Arthritis: A Comprehensive Guide
Osteoarthritis (OA) and rheumatoid arthritis (RA) are both forms of arthritis, causing pain and inflammation in the joints. However, they differ significantly in their underlying causes, the joints they affect, and their progression. Understanding these differences is crucial for appropriate diagnosis and management. This article delves deep into one key distinction: the underlying cause of joint damage. While other differences exist (such as the types of joints affected, the presence of systemic symptoms, and the response to treatment), focusing on the etiology provides a clear and foundational understanding of these two distinct conditions.
The Core Difference: Inflammation's Role
The primary difference between osteoarthritis and rheumatoid arthritis lies in the role of inflammation. While both conditions involve joint pain and stiffness, the inflammatory process is fundamentally different.
Osteoarthritis: A "Wear and Tear" Disease
Osteoarthritis, also known as degenerative joint disease, is primarily a non-inflammatory condition. The damage arises from the gradual breakdown of cartilage, the cushioning tissue between bones in a joint. Over time, this cartilage wears away, leading to bone-on-bone friction, pain, stiffness, and limited range of motion. While some inflammation might occur as a secondary response to the cartilage breakdown and bone spurs, it is not the primary driver of the disease process. Think of it like this: OA is like the gradual wear and tear on a car's engine – the parts slowly degrade with use.
Key features highlighting the non-inflammatory nature of OA:
- Cartilage Degradation: The primary issue is the progressive loss of articular cartilage.
- Bone Spurs (Osteophytes): The body attempts to compensate for cartilage loss by forming bone spurs, which can further restrict movement and cause pain.
- Limited Inflammation: While some inflammation can be present, it's usually a consequence of the mechanical damage, rather than the primary cause.
- Localized Symptoms: OA typically affects specific joints, often those bearing the most weight (hips, knees, spine).
- Gradual Onset: Symptoms usually develop slowly over time.
Rheumatoid Arthritis: A Systemic Autoimmune Disease
Rheumatoid arthritis, in stark contrast, is a systemic autoimmune disease. This means the body's own immune system mistakenly attacks the synovium, the lining of the joints. This attack triggers a chronic inflammatory response, leading to significant joint damage. The inflammation isn't just localized to the joint; it can affect other parts of the body, resulting in systemic symptoms. Imagine RA as a malfunctioning immune system attacking its own healthy tissue – the engine isn't just wearing out, it's being actively sabotaged.
Key features highlighting the inflammatory nature of RA:
- Synovitis: The inflammation of the synovial membrane is the hallmark of RA. This inflammation leads to swelling, pain, and eventual joint destruction.
- Pannus Formation: The inflamed synovium forms a layer of abnormal tissue called pannus, which invades and erodes the cartilage and bone.
- Extensive Inflammation: Inflammation is widespread, impacting not only the joints but also potentially other organs and tissues.
- Symmetrical Joint Involvement: RA often affects multiple joints symmetrically (e.g., both hands, both knees).
- Systemic Symptoms: Patients with RA frequently experience fatigue, fever, weight loss, and other systemic symptoms indicating the body's overall response to inflammation.
Comparing the Inflammatory Processes: A Closer Look
To further illustrate the difference, let's examine the inflammatory processes in more detail:
| Feature | Osteoarthritis (OA) | Rheumatoid Arthritis (RA) |
|---|---|---|
| Primary Cause | Cartilage degeneration, wear and tear | Autoimmune response, synovitis |
| Inflammation | Minimal, secondary to damage | Extensive, chronic, systemic |
| Joint Damage | Gradual, localized cartilage loss and bone spurs | Rapid, progressive, cartilage and bone destruction |
| Immune System | Not significantly involved | Directly involved, attacking the synovium |
| Systemic Effects | Usually absent | Often present (fatigue, fever, weight loss, etc.) |
| Onset | Gradual, insidious | Often rapid, with periods of flares and remission |
Beyond the Inflammatory Difference: Other Key Distinctions
While the difference in the inflammatory process forms the cornerstone of differentiating OA and RA, several other features help distinguish these conditions:
- Joint Involvement: OA typically affects weight-bearing joints (knees, hips, spine), while RA can affect many joints, including smaller joints of the hands and feet, symmetrically.
- Morning Stiffness: Morning stiffness is typically brief in OA (lasting less than 30 minutes), while it can last much longer (often an hour or more) in RA.
- Blood Tests: Blood tests, particularly rheumatoid factor (RF) and anti-citrullinated peptide antibodies (ACPA), are commonly used to support the diagnosis of RA. These are typically negative in OA.
- Imaging Studies: X-rays can show cartilage loss and bone spurs in OA, while in RA, they may reveal joint erosions and narrowing of the joint space.
- Treatment: Treatments for OA focus on pain management, improving joint function, and slowing disease progression. Treatments for RA aim to suppress the immune response and control inflammation, often involving disease-modifying antirheumatic drugs (DMARDs).
The Importance of Accurate Diagnosis
Accurately differentiating between OA and RA is crucial for effective treatment. While both conditions share symptoms like joint pain and stiffness, the underlying mechanisms and appropriate management strategies are vastly different. Misdiagnosis can lead to inappropriate treatment, delaying effective intervention and potentially worsening joint damage.
Consult a healthcare professional: If you experience persistent joint pain or stiffness, it's crucial to consult a doctor or rheumatologist for a proper diagnosis. They will conduct a thorough examination, review your medical history, and order relevant tests to determine the underlying cause of your symptoms.
Living with OA and RA: Strategies for Management
Managing both OA and RA requires a multifaceted approach:
Osteoarthritis Management:
- Pain Management: Over-the-counter pain relievers (like acetaminophen), topical analgesics, and in some cases, stronger prescription medications.
- Physical Therapy: Exercises to strengthen muscles, improve range of motion, and reduce pain.
- Weight Management: Maintaining a healthy weight reduces stress on weight-bearing joints.
- Assistive Devices: Canes, walkers, or other devices can improve mobility and reduce joint stress.
- Joint Replacement Surgery: In severe cases, joint replacement surgery might be considered.
Rheumatoid Arthritis Management:
- Disease-Modifying Antirheumatic Drugs (DMARDs): These medications help slow the progression of RA and reduce inflammation.
- Biologic Medications: These target specific parts of the immune system to reduce inflammation.
- Corticosteroids: These powerful anti-inflammatory drugs can provide rapid relief from symptoms.
- Physical Therapy: Similar to OA, physical therapy is crucial to maintain joint mobility and strength.
- Lifestyle Modifications: Stress management techniques, proper nutrition, and regular exercise can all play a role in managing RA.
Conclusion
The key difference between osteoarthritis and rheumatoid arthritis lies in the role of inflammation. OA is primarily a degenerative condition characterized by cartilage breakdown, while RA is a systemic autoimmune disease driven by chronic synovitis. Understanding this fundamental difference is crucial for accurate diagnosis and the implementation of appropriate and effective management strategies. While both conditions can cause significant pain and disability, early diagnosis and appropriate treatment can significantly improve quality of life for individuals affected by either OA or RA. Remember, consulting a healthcare professional is vital for a proper diagnosis and personalized treatment plan. This detailed comparison helps clarify the distinctions between these two prevalent forms of arthritis, empowering individuals and healthcare providers alike to provide optimal care.
Latest Posts
Latest Posts
-
Which Of The Following Corresponds To A Single Fascicle
Mar 25, 2025
-
Si La Puerta No Esta Abierta Esta
Mar 25, 2025
-
Two Emts Witnessed A Call In Which A Coworker
Mar 25, 2025
-
In This Excerpt Schlosser Claims That Fast Food Restaurants Are
Mar 25, 2025
-
The Family Care Plan Coordinator Reports Directly To What Person
Mar 25, 2025
Related Post
Thank you for visiting our website which covers about One Difference Between Osteoarthritis And Rheumatoid Arthritis Is That Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
