The Kidneys Are Stimulated To Produce Renin
Breaking News Today
Mar 22, 2025 · 6 min read
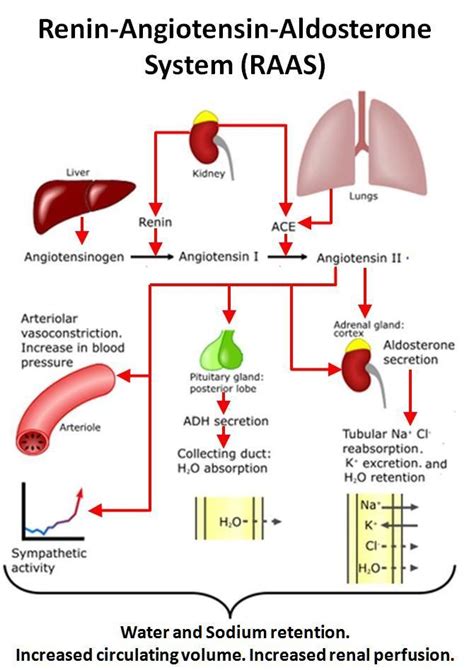
Table of Contents
The Kidneys are Stimulated to Produce Renin: A Deep Dive into the Renin-Angiotensin-Aldosterone System (RAAS)
The renin-angiotensin-aldosterone system (RAAS) is a crucial hormonal system that regulates blood pressure and fluid balance within the body. Central to this system is renin, an enzyme produced by the kidneys. Understanding the precise mechanisms that stimulate the kidneys to produce renin is vital for comprehending hypertension, heart failure, and other cardiovascular diseases. This comprehensive article explores the multifaceted stimuli that trigger renin release, delving into the intricate physiological processes involved.
The Primary Stimuli for Renin Release: A Detailed Examination
Several factors intricately interact to influence renin secretion. These stimuli can be broadly categorized as:
1. Reduced Renal Perfusion Pressure (RPP): The Baroreceptor Mechanism
This is arguably the most significant stimulus for renin release. Reduced renal perfusion pressure, meaning a decrease in the blood flow to the kidneys, activates the juxtaglomerular apparatus (JGA). The JGA, a specialized structure within the kidney, comprises cells that directly sense changes in blood pressure within the afferent arterioles. These specialized cells, known as granular cells, are the primary source of renin.
When renal perfusion pressure drops, the granular cells detect this decrease in pressure via baroreceptors, stretch-sensitive receptors within the afferent arterioles. This reduced stretch triggers a signaling cascade that ultimately leads to an increase in renin release. The mechanism involves several steps:
- Decreased stretch: The decreased blood flow causes less stretch on the afferent arterioles.
- Reduced calcium influx: The reduced stretch leads to decreased calcium influx into the granular cells.
- Depolarization of granular cells: Reduced calcium influx causes depolarization of the granular cells.
- Opening of voltage-gated calcium channels: This depolarization opens voltage-gated calcium channels.
- Calcium influx and exocytosis: Increased calcium influx triggers exocytosis, the process of releasing renin from storage granules within the granular cells.
This intricate mechanism ensures that when blood pressure falls, the kidneys respond by releasing renin, initiating a chain reaction to restore blood pressure to normal levels. This is a crucial homeostatic mechanism preventing potentially dangerous hypotension.
2. Sympathetic Nervous System Activation: Norepinephrine's Role
The sympathetic nervous system, part of the autonomic nervous system, plays a significant role in regulating blood pressure. Activation of the sympathetic nervous system, often in response to stress or decreased blood volume, stimulates renin release.
The sympathetic nervous system innervates the juxtaglomerular apparatus, releasing norepinephrine. Norepinephrine binds to β1-adrenergic receptors on the granular cells. This binding triggers a cascade of intracellular events leading to increased renin secretion. The mechanism differs slightly from the baroreceptor mechanism:
- Norepinephrine binding: Norepinephrine binds to β1-adrenergic receptors on the granular cells.
- Activation of adenylate cyclase: This binding activates adenylate cyclase.
- Increased cAMP levels: This leads to an increase in cyclic adenosine monophosphate (cAMP) levels within the granular cells.
- Calcium influx and exocytosis: Increased cAMP levels enhance calcium influx and stimulate exocytosis, resulting in renin release.
This pathway provides a rapid response to situations demanding increased blood pressure, complementing the slower baroreceptor mechanism.
3. Decreased Sodium Chloride Delivery to the Distal Tubule: The Macula Densa Feedback Mechanism
The macula densa, another crucial component of the JGA, senses the sodium chloride (NaCl) concentration in the distal tubule. A decrease in NaCl delivery to the macula densa, often reflecting reduced renal perfusion pressure or decreased extracellular fluid volume, also stimulates renin release.
This mechanism is a complex feedback loop:
- Reduced NaCl delivery: Decreased renal perfusion or extracellular fluid volume leads to a reduction in NaCl delivery to the macula densa.
- Signal to granular cells: The macula densa cells detect this reduction and send a signal to the granular cells.
- Renin release: The exact nature of the signal remains a subject of ongoing research, but it likely involves paracrine signaling molecules, such as adenosine and prostaglandins, leading to increased renin secretion.
This macula densa feedback mechanism acts as a fine-tuner, ensuring a proportionate renin release based on the ongoing renal sodium and fluid status.
The Consequences of Renin Release: The RAAS Cascade
The release of renin initiates a cascade of events involving several key players:
- Renin converts angiotensinogen to angiotensin I: Renin, released from the granular cells, acts on angiotensinogen, a protein produced in the liver, converting it to angiotensin I.
- Angiotensin-converting enzyme (ACE) converts angiotensin I to angiotensin II: Angiotensin I is then converted to angiotensin II by ACE, an enzyme primarily found in the lungs.
- Angiotensin II's effects: Angiotensin II is a potent vasoconstrictor, raising blood pressure directly by constricting blood vessels. It also stimulates the adrenal cortex to release aldosterone.
- Aldosterone's effects: Aldosterone acts on the kidneys, increasing sodium reabsorption and potassium excretion. This increase in sodium reabsorption leads to increased water retention, further raising blood volume and blood pressure.
Clinical Significance of Understanding Renin Release
Understanding the mechanisms that stimulate renin release is crucial in managing several clinical conditions:
- Hypertension: In many forms of hypertension, the RAAS is overactive, leading to excessive vasoconstriction and fluid retention. Drugs that inhibit different components of the RAAS, such as ACE inhibitors and angiotensin receptor blockers (ARBs), are commonly used to treat hypertension.
- Heart Failure: Heart failure often leads to reduced renal perfusion pressure, stimulating renin release. This contributes to fluid retention and worsening of heart failure symptoms. RAAS inhibitors are also frequently used in heart failure management.
- Kidney Diseases: Kidney diseases can disrupt the normal function of the JGA, leading to abnormal renin secretion. This can contribute to complications such as hypertension and fluid imbalances.
- Hypovolemia: Conditions causing low blood volume, such as dehydration or hemorrhage, trigger increased renin secretion as the body attempts to restore blood volume and pressure.
Future Directions and Ongoing Research
Despite extensive research, many aspects of renin regulation remain to be fully elucidated. Ongoing research focuses on:
- Clarifying the precise signaling pathways within the JGA: The precise signaling molecules and intracellular mechanisms involved in the communication between the macula densa and granular cells require further investigation.
- Investigating the role of other factors: Other factors, such as nitric oxide, prostaglandins, and other hormones, are likely to modulate renin secretion, but their precise roles require further study.
- Developing novel therapeutic strategies: A deeper understanding of renin regulation could lead to the development of more effective treatments for hypertension, heart failure, and other cardiovascular diseases.
Conclusion
The kidneys' production of renin is a tightly regulated process involving multiple complex mechanisms. The primary stimuli—reduced renal perfusion pressure, sympathetic nervous system activation, and decreased sodium chloride delivery to the distal tubule—work in concert to maintain blood pressure and fluid homeostasis. Disruptions in this intricate system can lead to various cardiovascular diseases, highlighting the importance of understanding these mechanisms for both diagnosis and treatment. Ongoing research continues to unravel the intricacies of renin regulation, paving the way for improved therapeutic strategies in the future. This comprehensive overview provides a robust foundation for further exploration into this essential physiological process.
Latest Posts
Latest Posts
-
How Are Stress And Physical Health Related Quizlet
Mar 23, 2025
-
You Notice The Person Giving Chest Compressions Quizlet
Mar 23, 2025
-
Scope And Standards Of Practice Ati Quizlet
Mar 23, 2025
-
Genital Warts Are Spread To Others By Quizlet
Mar 23, 2025
-
The Condensate Drain On A Rooftop Unit Quizlet
Mar 23, 2025
Related Post
Thank you for visiting our website which covers about The Kidneys Are Stimulated To Produce Renin . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
