The Systematic Head To Toe Assessment Should Be Performed On
Breaking News Today
Apr 01, 2025 · 6 min read
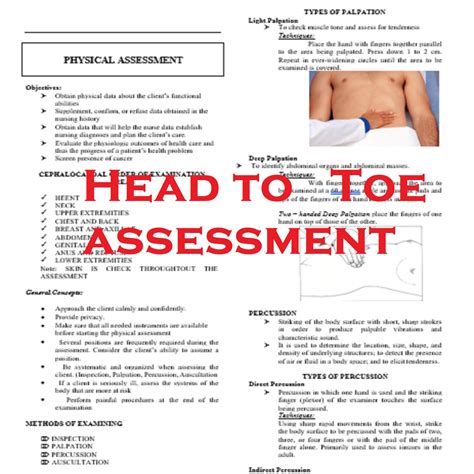
Table of Contents
The Systematic Head-to-Toe Assessment: A Comprehensive Guide for Healthcare Professionals
Performing a thorough head-to-toe assessment is a fundamental skill for all healthcare professionals, from nurses and paramedics to physicians and physician assistants. This systematic approach allows for a comprehensive evaluation of a patient's overall health status, identifying both obvious and subtle signs and symptoms of various conditions. This in-depth guide explores the process, highlighting key aspects and considerations for each body region. Mastering this technique is crucial for early diagnosis, effective treatment planning, and ultimately, improved patient outcomes.
Why Perform a Head-to-Toe Assessment?
A systematic head-to-toe assessment serves several crucial purposes:
-
Early Detection of Problems: It enables the early detection of abnormalities, allowing for prompt intervention and preventing complications. Many conditions present with subtle signs initially, easily missed during a less comprehensive examination.
-
Comprehensive Health Overview: It provides a holistic picture of the patient's health, considering interconnected systems and potential underlying causes. Symptoms often manifest across multiple body systems.
-
Baseline Data Collection: It establishes a baseline for future comparisons. Tracking changes over time is crucial in monitoring disease progression or response to treatment.
-
Patient Safety: Identifying potential risks and hazards ensures patient safety, especially in acutely ill patients.
-
Legal Protection: A well-documented head-to-toe assessment provides legal protection for healthcare providers, demonstrating due diligence and adherence to professional standards of care.
The Systematic Approach: A Step-by-Step Guide
The head-to-toe assessment follows a structured sequence, progressing logically from head to toe. This ensures no area is overlooked and maximizes efficiency. While the specific order may vary slightly based on the healthcare setting and individual patient needs, the core components remain consistent. Remember to always maintain patient privacy and comfort throughout the assessment.
1. General Appearance and Vital Signs: Setting the Stage
Before beginning the detailed physical examination, observe the patient's general appearance. Note their level of consciousness, alertness, and overall demeanor. Are they anxious, distressed, or comfortable? This initial observation often provides valuable clues about their overall health.
Key observations:
- Level of consciousness (LOC): Alert, drowsy, lethargic, stuporous, comatose. Utilize the Glasgow Coma Scale (GCS) if necessary.
- Mental status: Orientation to person, place, and time. Assess cognitive function if concerns arise.
- Body language and affect: Posture, facial expression, mood.
- Skin color and temperature: Note any pallor, cyanosis, jaundice, or unusual warmth or coolness.
- Nutritional status: Apparent weight loss or gain.
- Hygiene: Assess personal cleanliness.
Vital signs are crucial:
- Temperature: Oral, rectal, axillary, or tympanic.
- Pulse: Rate, rhythm, strength.
- Respirations: Rate, rhythm, depth.
- Blood pressure: Systolic and diastolic readings.
- Oxygen saturation (SpO2): Using pulse oximetry.
- Pain assessment: Using a standardized pain scale (e.g., numerical rating scale, visual analog scale).
2. Head and Neck: Neurological and Sensory Assessment
This section focuses on neurological function, cranial nerves, and the integrity of the head and neck structures.
Key assessment points:
- Head: Inspect for symmetry, lesions, masses, or tenderness. Palpate the scalp.
- Eyes: Assess visual acuity (using a Snellen chart or similar), pupillary response (PERRLA – pupils equal, round, reactive to light and accommodation), extraocular movements (EOMs), and conjunctiva and sclera for redness or jaundice.
- Ears: Assess hearing acuity (whispered voice test or finger rub), inspect the external ear canal for cerumen or lesions.
- Nose: Assess patency of nasal passages, inspect for nasal discharge or deformities.
- Mouth and throat: Inspect the lips, oral mucosa, teeth, tongue, and pharynx for lesions, inflammation, or abnormalities. Assess gag reflex.
- Neck: Palpate lymph nodes for enlargement or tenderness. Assess range of motion (ROM) of the neck. Auscultate the carotid arteries for bruits. Inspect the jugular venous pressure (JVP).
3. Chest and Lungs: Respiratory System Evaluation
The chest assessment focuses on the respiratory system, including the lungs and heart.
Key assessment points:
- Inspection: Observe respiratory rate and rhythm, chest wall symmetry, and use of accessory muscles.
- Palpation: Assess chest expansion, tactile fremitus (vibrations felt during speech), and tenderness.
- Percussion: Assess lung resonance and identify areas of dullness or hyperresonance.
- Auscultation: Listen for breath sounds (vesicular, bronchial, bronchovesicular), adventitious sounds (crackles, wheezes, rhonchi, pleural rubs), and heart sounds.
4. Cardiovascular System: Heart and Vessels
This section assesses the cardiovascular system, focusing on the heart and blood vessels.
Key assessment points:
- Inspection: Observe for jugular venous distention (JVD), precordial heaves or lifts.
- Palpation: Palpate the apical impulse and assess for thrills or heaves.
- Auscultation: Listen for heart sounds (S1, S2, S3, S4, murmurs), assess rate and rhythm. Auscultate peripheral pulses for strength and regularity. Assess capillary refill time.
5. Abdomen: Gastrointestinal System
A thorough abdominal assessment examines the gastrointestinal system and other abdominal organs.
Key assessment points:
- Inspection: Observe abdominal contour, distention, scars, and visible pulsations.
- Auscultation: Listen for bowel sounds in all four quadrants.
- Percussion: Assess for tympany and dullness.
- Palpation: Gently palpate all four quadrants, noting tenderness, masses, or organomegaly.
6. Musculoskeletal System: Strength and Mobility
Assess the patient's musculoskeletal system to identify any abnormalities.
Key assessment points:
- Inspection: Observe posture, gait, and range of motion (ROM) of all joints. Note any deformities, swelling, or redness.
- Palpation: Assess muscle tone, strength, and tenderness. Palpate joints for warmth, swelling, or crepitus.
- Range of motion testing: Assess active and passive ROM in all joints.
7. Neurological System: Function and Reflexes
A neurological assessment should evaluate both cranial nerves and peripheral neurological function.
Key assessment points:
- Mental status: Already assessed earlier, but reassess if indicated.
- Cranial nerves: Assess function of each cranial nerve (I-XII).
- Motor function: Assess muscle strength, tone, and coordination.
- Sensory function: Assess light touch, pain, temperature, and proprioception.
- Reflexes: Assess deep tendon reflexes (DTRs) and superficial reflexes.
8. Skin: Integrity and Lesions
A skin assessment is essential for identifying skin abnormalities and potential underlying conditions.
Key assessment points:
- Inspection: Observe skin color, moisture, temperature, and texture. Note any lesions, rashes, or wounds.
- Palpation: Assess skin turgor (hydration status).
9. Peripheral Vascular System: Circulation Assessment
This assessment focuses on the circulation in the extremities.
Key assessment points:
- Inspection: Observe for edema, discoloration, or ulcerations.
- Palpation: Assess peripheral pulses (radial, brachial, femoral, popliteal, posterior tibial, dorsalis pedis) for strength and regularity. Assess skin temperature and capillary refill time.
10. Genitourinary System: Examination as Needed
This is conducted based on the patient's condition and clinical presentation. It may include inspection of the external genitalia and assessment of urinary function.
11. Documentation: A Crucial Step
Thorough documentation is paramount. Record all findings accurately and objectively. Use standardized terminology and include specific measurements and observations. This ensures continuity of care and facilitates communication among healthcare professionals.
Conclusion: A Vital Skill for Healthcare Professionals
The systematic head-to-toe assessment is a cornerstone of patient care. Its systematic nature ensures comprehensiveness and helps prevent oversight. By consistently utilizing this approach, healthcare professionals can identify potential problems early, optimize treatment strategies, and significantly improve patient outcomes. Remember, ongoing education and practice are essential for refining this vital skill and maintaining a high standard of patient care. Continuous learning and engagement with the ever-evolving medical landscape are crucial for any healthcare professional. This holistic approach to assessment helps ensure that you are providing the most comprehensive and effective care possible.
Latest Posts
Latest Posts
-
Amoeba Sisters Video Recap Answer Key Cell Transport
Apr 02, 2025
-
What Does Extension Of A Point Refer To
Apr 02, 2025
-
Decidimos Venir A Este Restaurante Porque Mi Jefe
Apr 02, 2025
-
Skills Module 3 0 Intravenous Medication Administration Posttest
Apr 02, 2025
-
America The Story Of Us Episode 9 Bust
Apr 02, 2025
Related Post
Thank you for visiting our website which covers about The Systematic Head To Toe Assessment Should Be Performed On . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
