Tina Jones Comprehensive Assessment Shadow Health Subjective
Breaking News Today
Mar 25, 2025 · 6 min read
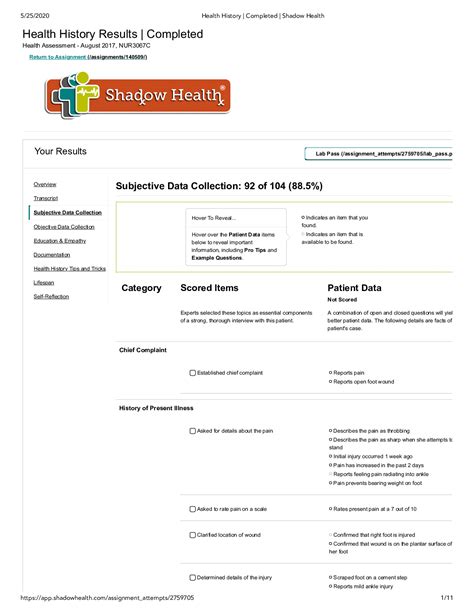
Table of Contents
Tina Jones Comprehensive Assessment: A Deep Dive into Shadow Health's Subjective Data
Shadow Health's Tina Jones comprehensive assessment provides nursing students with a realistic simulation to practice crucial patient interaction and data gathering skills. This detailed exploration delves into the subjective data gathered during this virtual encounter, emphasizing the importance of active listening, thorough questioning, and accurate documentation. We'll examine key findings, potential diagnoses, and the crucial role of subjective information in forming a comprehensive patient picture.
Understanding the Subjective Data Gathering Process
The subjective portion of a patient assessment relies heavily on the patient's self-reported information. This includes their feelings, symptoms, perceptions, and history. In the Tina Jones simulation, effective data gathering requires mastering several key techniques:
Active Listening:
Active listening goes beyond simply hearing the patient's words. It involves paying close attention to their verbal and nonverbal cues, asking clarifying questions, and reflecting back what you've heard to ensure understanding. In Tina Jones' case, noticing her hesitations, tone of voice, and body language can provide valuable insights beyond her spoken words.
Open-Ended Questions:
Instead of using closed-ended questions that elicit simple "yes" or "no" answers, open-ended questions encourage patients to elaborate. For example, instead of asking "Do you have pain?", a better approach is "Can you describe the pain you're experiencing?". This allows for a richer understanding of the patient's experience.
Clarifying and Probing:
It's crucial to clarify any ambiguous statements and probe for deeper understanding. If Tina Jones mentions feeling "stressed," follow up with questions about the sources of her stress, its duration, and its impact on her daily life.
Building Rapport:
Establishing a trusting relationship with the patient is vital for obtaining accurate and complete subjective data. A warm, empathetic approach can encourage Tina Jones to open up and share more readily.
Tina Jones' Subjective Data: A Detailed Analysis
Tina Jones' subjective data in the Shadow Health simulation covers several key areas:
Chief Complaint:
Tina Jones presents with a chief complaint of severe headaches, nausea, and vomiting for the past three days. This immediately signals the need for a thorough investigation into the underlying cause. The severity and duration of her symptoms require immediate attention.
Present Illness:
The description of her present illness should include detailed information about the onset, location, character, radiation, associated symptoms, timing, exacerbating factors, relieving factors, and severity (OLDCARTS). For example:
- Onset: When did the headaches start? Three days ago.
- Location: Where is the headache? Describing the location precisely (e.g., frontal, occipital, bilateral) is important.
- Character: How would she describe the pain? Sharp, dull, throbbing, etc.
- Radiation: Does the pain radiate anywhere else?
- Associated Symptoms: Nausea and vomiting are key associated symptoms, pointing towards a possible migraine or other serious condition. Fever, visual disturbances, or neurological symptoms need to be explored.
- Timing: How often do the headaches occur? Are they constant or intermittent?
- Exacerbating Factors: What makes the headaches worse? Stress, light, sounds, etc.
- Relieving Factors: What makes the headaches better? Rest, medication, dark room?
- Severity: On a scale of 1 to 10, how severe is the pain?
The detailed exploration of these aspects of her present illness is crucial for differential diagnosis.
Past Medical History:
Tina Jones' past medical history is equally important. This section should include information about previous illnesses, surgeries, hospitalizations, allergies, and current medications. The presence of any conditions that might contribute to her current symptoms (e.g., hypertension, migraines) needs to be carefully documented. Any history of head trauma is also crucial.
Family History:
A comprehensive family history is essential in identifying potential genetic predispositions to certain conditions. Inquiring about family history of migraines, headaches, hypertension, or other relevant medical conditions can provide valuable insights.
Social History:
Social history encompasses factors that can influence health, such as lifestyle, occupation, and relationships. Key aspects to explore in Tina Jones' case include:
- Smoking: Does she smoke? If so, how many cigarettes per day?
- Alcohol consumption: Does she drink alcohol? If so, how much and how often?
- Drug use: Does she use any recreational drugs?
- Diet: What is her typical diet like?
- Exercise: How much physical activity does she get?
- Stress levels: How would she describe her stress levels?
- Sleep patterns: How many hours of sleep does she get per night?
- Occupation: What is her job? Are there any potential occupational hazards that could contribute to her symptoms?
- Support system: Does she have a supportive social network?
Review of Systems (ROS):
A systematic review of systems explores various body systems to identify any other potential problems. While Tina Jones' chief complaint focuses on the neurological system, it's crucial to assess other systems to rule out other possibilities. This includes investigating symptoms related to:
- Neurological: Any other neurological symptoms such as dizziness, weakness, numbness, tingling, vision changes, or loss of consciousness?
- Cardiovascular: Chest pain, palpitations, shortness of breath?
- Respiratory: Cough, shortness of breath, wheezing?
- Gastrointestinal: Any other gastrointestinal issues beyond nausea and vomiting? Appetite changes, abdominal pain, diarrhea, constipation?
- Genitourinary: Any changes in urination?
- Musculoskeletal: Muscle aches, joint pain, stiffness?
- Integumentary: Rashes, skin changes?
- Psychosocial: Mood changes, anxiety, depression, stress?
Interpreting Subjective Data and Differential Diagnoses
Synthesizing Tina Jones' subjective data allows for the formulation of a differential diagnosis – a list of possible conditions that could be causing her symptoms. Based on the information gathered, potential diagnoses might include:
- Migraine headache: The combination of severe headache, nausea, and vomiting strongly suggests this possibility.
- Tension headache: While less likely given the severity and associated symptoms, this remains a differential diagnosis.
- Sinusitis: If there are facial pain and pressure symptoms, sinusitis should be considered.
- Other neurological conditions: Depending on the specifics of her symptoms and ROS, other neurological conditions might need to be explored.
The Importance of Subjective Data in Patient Care
The subjective data gathered from Tina Jones forms the foundation of her assessment. It's crucial for several reasons:
- Patient-centered care: It allows for a deep understanding of the patient's experience, leading to more effective and personalized treatment plans.
- Early diagnosis: Accurate and thorough subjective data can lead to earlier diagnosis and intervention, improving patient outcomes.
- Building trust and rapport: Effective communication and active listening foster trust between the healthcare provider and the patient, encouraging better adherence to treatment plans.
- Comprehensive assessment: Subjective data, combined with objective data from the physical examination, laboratory tests, and other diagnostic tools, paints a complete picture of the patient's health.
Conclusion: Mastering the Art of Subjective Data Gathering
The Tina Jones simulation in Shadow Health provides an invaluable opportunity to practice the essential skill of gathering comprehensive subjective data. By mastering active listening, using open-ended questions, clarifying ambiguities, and building rapport, nursing students can develop the critical skills needed to provide high-quality, patient-centered care. Thorough documentation of subjective data is paramount for accurate diagnosis, effective treatment planning, and ultimately, improved patient outcomes. The careful consideration of all aspects of Tina Jones’ experience, from her chief complaint to her psychosocial history, demonstrates a commitment to holistic patient assessment and highlights the critical role of subjective information in the decision-making process. The ability to effectively elicit and interpret subjective data is foundational to competent nursing practice.
Latest Posts
Latest Posts
Related Post
Thank you for visiting our website which covers about Tina Jones Comprehensive Assessment Shadow Health Subjective . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
