What Causes Hemolytic Disease Of The Newborn Quizlet
Breaking News Today
Mar 24, 2025 · 5 min read
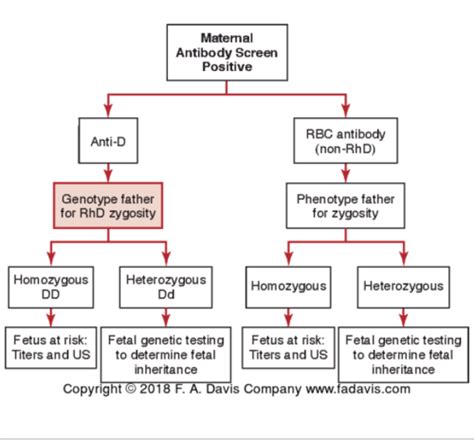
Table of Contents
What Causes Hemolytic Disease of the Newborn? A Comprehensive Guide
Hemolytic disease of the newborn (HDN), also known as erythroblastosis fetalis, is a condition affecting the fetus or newborn infant. It occurs when the mother's immune system produces antibodies that attack the red blood cells of her baby. This destruction of red blood cells, known as hemolysis, can lead to various health complications, ranging from mild jaundice to severe anemia and even death. Understanding the underlying causes is crucial for effective prevention and management.
The Role of Blood Group Incompatibility
The primary cause of HDN is blood group incompatibility between the mother and her baby. This incompatibility most commonly involves the Rh factor and, less frequently, the ABO blood group system.
Rh Incompatibility: The Most Common Culprit
The Rh factor is a protein found on the surface of red blood cells. Individuals are either Rh-positive (Rh+) if they have this protein or Rh-negative (Rh-) if they don't. Problems arise when an Rh-negative mother carries an Rh-positive fetus.
-
Sensitization: During pregnancy, or especially during delivery, some of the baby's Rh-positive blood cells may enter the mother's bloodstream. This exposure sensitizes the mother's immune system, causing her body to produce anti-Rh antibodies. These antibodies cross the placenta and attack the baby's Rh-positive red blood cells.
-
Subsequent Pregnancies: The risk of HDN increases with each subsequent pregnancy involving an Rh-positive fetus. The mother's already-existing anti-Rh antibodies are readily available to cross the placenta and attack the fetal red blood cells, causing more significant hemolysis. The first pregnancy typically shows mild or no symptoms because antibody production takes time.
ABO Incompatibility: A Less Severe, Yet Significant Cause
ABO incompatibility occurs when the mother has a different ABO blood group than the baby. For example, an O-negative mother carrying an A-positive or B-positive baby can develop ABO HDN.
-
Natural Antibodies: Unlike Rh incompatibility, where sensitization is required, mothers with blood type O already possess naturally occurring antibodies against A and B antigens. These antibodies, though typically weaker than Rh antibodies, can still cross the placenta and attack the fetal red blood cells.
-
Less Severe Effects: Generally, ABO incompatibility leads to a milder form of HDN than Rh incompatibility. However, it still poses a risk, especially for infants with blood type A or B.
Other Factors Contributing to HDN Severity
While blood group incompatibility is the main cause, several other factors influence the severity of HDN:
-
Antibody titer: The concentration of maternal antibodies directly impacts the extent of hemolysis. Higher antibody titers indicate a greater risk of severe HDN.
-
Placental transfer: The efficiency of antibody transfer across the placenta varies. A more permeable placenta can allow more antibodies to reach the fetus, leading to more severe disease.
-
Fetal red blood cell destruction rate: Individual differences in the rate at which fetal red blood cells are destroyed affect the severity of the condition. Some fetuses are more susceptible to hemolysis.
-
Gestational age: HDN can manifest at different gestational ages. Severe cases may present earlier in pregnancy.
Diagnosing Hemolytic Disease of the Newborn
Early and accurate diagnosis is crucial for effective management. Several tests are employed to detect HDN:
-
Maternal antibody screening: This blood test is performed routinely during pregnancy to detect the presence of antibodies.
-
Ultrasound: This imaging technique helps assess the size of the fetus and the amount of amniotic fluid. An increased amount of fluid can be a sign of HDN.
-
Amniocentesis: This procedure involves extracting amniotic fluid to measure bilirubin levels. High bilirubin levels suggest increased red blood cell destruction.
-
Percutaneous umbilical blood sampling (PUBS): This involves sampling fetal blood from the umbilical cord to determine the severity of anemia.
Treatment Options for Hemolytic Disease of the Newborn
Treatment strategies depend on the severity of the condition and the gestational age. Options include:
-
Intrauterine transfusion: In severe cases, a blood transfusion is performed directly into the fetus while still in the womb. This helps alleviate anemia and improve survival chances.
-
Phototherapy: After birth, phototherapy, which involves exposing the baby to special lights, is used to break down bilirubin. This reduces the risk of jaundice-related complications.
-
Exchange transfusion: This procedure involves replacing the baby's affected blood with healthy donor blood. This is a more extensive procedure to address severe anemia and high bilirubin levels.
-
Supportive care: This encompasses measures such as monitoring vital signs, fluid management, and providing respiratory support, as needed.
Prevention of Hemolytic Disease of the Newborn
Preventing HDN is far preferable to treating it. The most effective prevention strategy is the administration of Rho(D) immune globulin (RhoGAM).
-
RhoGAM administration: This injection contains antibodies that prevent the mother's immune system from producing anti-Rh antibodies. It is typically given to Rh-negative mothers at 28 weeks of gestation and again within 72 hours after delivery if the baby is Rh-positive. It may also be given after certain procedures, such as amniocentesis or miscarriage.
-
Early identification of risk: Accurate blood typing and antibody screening during pregnancy are essential for identifying women at risk for HDN.
-
Careful monitoring: Regular monitoring during pregnancy and close observation of the newborn can help detect and manage HDN effectively.
Long-Term Effects of Hemolytic Disease of the Newborn
The long-term effects of HDN vary depending on the severity of the condition and the effectiveness of treatment. In many cases, with appropriate intervention, there are no lasting consequences. However, severe cases can potentially lead to:
-
Neurological damage: High bilirubin levels can lead to kernicterus, a type of brain damage that can cause hearing loss, cerebral palsy, and intellectual disability.
-
Developmental delays: Severe anemia and associated complications may affect the baby's cognitive and motor development.
-
Anemia: While usually corrected through treatment, severe anemia can have potential long-term effects, though this is rare with proper management.
Conclusion: A Comprehensive Understanding is Key
Hemolytic disease of the newborn is a complex condition stemming from blood group incompatibility. Understanding the underlying causes, diagnostic methods, treatment options, and preventive measures is crucial for optimizing maternal and neonatal outcomes. Early identification, proactive management, and advancements in medical care greatly improve the prognosis for affected infants. While the condition can be serious, early detection and timely intervention can significantly reduce the risk of long-term complications, ensuring the health and well-being of both mother and child. Continued research and awareness remain key to further improving outcomes in cases of HDN.
Latest Posts
Latest Posts
-
Where Can You Pin Frequently Used Apps For Easy Access
Mar 26, 2025
-
T Cells Achieve Self Tolerance In The
Mar 26, 2025
-
Define The Following Terms Close Up Portraiture Straight Photography
Mar 26, 2025
-
Which Of The Following Statements Is True About Alzheimers Disease
Mar 26, 2025
-
How Can Solar Irradiance Cause Coral Bleaching
Mar 26, 2025
Related Post
Thank you for visiting our website which covers about What Causes Hemolytic Disease Of The Newborn Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
