Which Is A Stroke Severity Tool That Helps Ems
Breaking News Today
Mar 16, 2025 · 6 min read
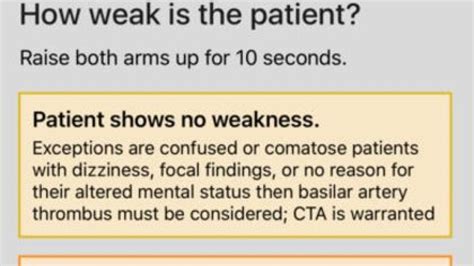
Table of Contents
Which Stroke Severity Tool Helps EMS? Understanding the Cincinnati Prehospital Stroke Scale and Beyond
Emergency Medical Services (EMS) personnel are on the front lines of stroke care, facing the critical challenge of rapidly assessing stroke severity and initiating timely interventions. Accurate and efficient stroke severity assessment is crucial for optimizing patient outcomes, as rapid treatment within the crucial therapeutic window is essential for minimizing long-term disability. While several tools exist, the Cincinnati Prehospital Stroke Scale (CPSS) remains a widely used and readily accessible option for prehospital stroke assessment. This article delves into the CPSS, its limitations, and explores other tools that are emerging to improve stroke identification and management in the prehospital setting.
The Cincinnati Prehospital Stroke Scale (CPSS): A Quick Overview
The CPSS is a simple, three-component neurological examination designed to quickly identify patients who may be experiencing an ischemic stroke. Its ease of use and minimal equipment requirements make it ideal for EMS professionals working in various settings and conditions. The three components are:
1. Facial Droop:
This assesses for asymmetry in facial expression. EMS personnel ask the patient to smile. A drooping or asymmetry of one side of the face compared to the other strongly suggests a stroke.
2. Arm Drift:
This evaluates upper extremity weakness. The patient is asked to close their eyes and extend both arms forward. Drift of one arm downward indicates potential stroke.
3. Speech:
This assesses for aphasia or dysarthria. EMS personnel ask the patient to repeat a simple phrase, such as "The sky is blue." Slurred speech or an inability to repeat the phrase points towards a possible stroke.
Scoring: Each of the three components is scored as either "normal" or "abnormal." The presence of any one abnormal finding warrants further evaluation and prioritization for stroke center transport. While the CPSS provides a rapid screening, it’s crucial to understand its limitations.
Limitations of the CPSS: Why it’s Not a Definitive Diagnostic Tool
While the CPSS provides a valuable initial screening, it's not a definitive diagnostic tool for stroke. Several limitations must be considered:
-
False Positives: The CPSS can yield false positives. Conditions such as Bell's palsy, anxiety, or other neurological conditions can mimic stroke symptoms, leading to unnecessary transport to a stroke center.
-
False Negatives: Conversely, the CPSS can also produce false negatives, meaning that some individuals experiencing a stroke might not display any of the three classic signs. This is particularly true in minor strokes or strokes affecting less visible areas of the brain.
-
Lack of Sensitivity and Specificity: The CPSS has limited sensitivity and specificity compared to more sophisticated diagnostic tools. Sensitivity refers to the ability of a test to correctly identify those with the disease, while specificity refers to the ability of a test to correctly identify those without the disease. A low sensitivity means that some individuals with a stroke may be missed, while a low specificity means that many individuals without a stroke might be misclassified as having one.
-
Subjectivity: The assessment relies on subjective interpretation, making the results potentially influenced by the EMS provider's experience and training. Inter-rater reliability might vary among different EMS teams.
-
Doesn't Assess Severity: The CPSS only identifies the potential presence of a stroke; it does not provide information on the severity of the stroke. This information is critical in determining treatment priorities and resource allocation.
-
Does Not Differentiate Stroke Types: It does not differentiate between ischemic stroke (the most common type) and hemorrhagic stroke.
Beyond the CPSS: Newer and More Comprehensive Stroke Severity Tools for EMS
Recognizing the limitations of the CPSS, researchers and clinicians continue to develop more sophisticated tools for prehospital stroke assessment. These newer tools aim to improve accuracy, sensitivity, and specificity. While not universally adopted, some show promise:
1. The Los Angeles Prehospital Stroke Screen (LAPSS): This scale incorporates additional neurological assessments beyond the CPSS, increasing its sensitivity and specificity. It includes questions about the patient's history, symptoms, and level of consciousness.
2. The Prehospital Stroke Scale (PHSS): A modified and expanded version of the CPSS, this aims for increased sensitivity, often incorporating elements like age, symptom duration, and past medical history.
3. Advanced Telemedicine Technology: The integration of telemedicine into prehospital care is revolutionizing stroke assessment. Real-time video consultations with stroke specialists allow for remote neurological examinations, potentially facilitating more accurate diagnoses and reducing false positives/negatives.
4. Point-of-Care Testing (POCT): POCT devices are emerging that can provide rapid blood tests for biomarkers associated with stroke, such as D-dimer. This can help differentiate between ischemic and hemorrhagic strokes, guiding treatment decisions.
The Importance of Ongoing Training and Education for EMS Professionals
Regardless of the specific tool utilized, ongoing training and education are crucial for EMS professionals. Continuous learning keeps them up-to-date on the latest advancements in stroke recognition and management. This training should encompass:
-
Refresher courses on using and interpreting stroke assessment tools.
-
Hands-on practice with various assessment methods.
-
Case studies and scenarios that highlight both common and atypical stroke presentations.
-
Discussions on ethical considerations and decision-making in prehospital stroke care.
-
Understanding the latest research and advancements in stroke treatment.
The Role of Technology in Improving Prehospital Stroke Care
Technology plays an increasingly important role in improving prehospital stroke care. Mobile applications can guide EMS personnel through the assessment process, provide immediate access to guidelines, and streamline communication with stroke centers.
Integrating digital tools that can:
-
Provide real-time feedback and guidance during the assessment.
-
Facilitate electronic transfer of patient data to stroke centers.
-
Allow for remote consultations with stroke specialists.
-
Support continuous monitoring of patients' vital signs and neurological status.
This enhanced data collection and communication facilitates more informed decision-making, potentially reducing delays in treatment and improving patient outcomes.
Conclusion: A Multifaceted Approach to Prehospital Stroke Care
While the Cincinnati Prehospital Stroke Scale remains a widely used tool, its limitations necessitate a multifaceted approach to prehospital stroke care. EMS personnel need to be equipped with comprehensive training, access to updated tools (including newer scales and technology), and consistent support for accurate assessment and timely interventions. The development and adoption of more sensitive and specific assessment tools, coupled with ongoing training and the integration of technology, are key to optimizing prehospital stroke care and maximizing positive patient outcomes. The ultimate goal is to minimize the impact of stroke, allowing individuals to recover as fully as possible. By continuously striving for improved accuracy in assessment and efficient management, we pave the way toward a future where even more lives can be positively impacted by swift and effective prehospital stroke intervention. The ongoing development and application of new technologies and refined assessment scales will continue to refine this essential area of emergency medicine.
Latest Posts
Latest Posts
-
Life Insurance Exam Questions And Answers Pdf
Mar 18, 2025
-
The Direct Carry Is Used To Transfer A Patient
Mar 18, 2025
-
The Emancipation Proclamation Of January 1 1863 Quizlet
Mar 18, 2025
-
These Cards Will Get You Drunk Quizlet
Mar 18, 2025
-
Did Quizlet Get Rid Of Q Chat
Mar 18, 2025
Related Post
Thank you for visiting our website which covers about Which Is A Stroke Severity Tool That Helps Ems . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
