Which Of The Following Examples Below Describes An Autoimmune Disease
Breaking News Today
Mar 21, 2025 · 7 min read
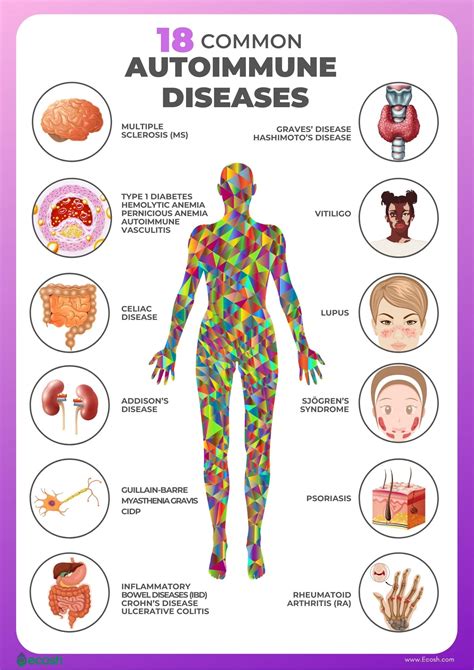
Table of Contents
Which of the Following Examples Describes an Autoimmune Disease?
Autoimmune diseases are a complex group of conditions where the body's immune system mistakenly attacks its own healthy tissues and organs. This self-attack can lead to a wide range of symptoms and health problems, depending on which organs or tissues are affected. Understanding what constitutes an autoimmune disease is crucial for both diagnosis and management. Let's delve into the characteristics of these diseases and explore several examples to clarify the concept.
Understanding the Immune System and Autoimmunity
Before examining specific examples, it's essential to grasp the basics of the immune system and how it malfunctions in autoimmune diseases. The immune system is a complex network of cells, tissues, and organs that work together to protect the body from foreign invaders like bacteria, viruses, and parasites. This defense mechanism relies on identifying and neutralizing these threats.
Key players in the immune system include:
- White blood cells (leukocytes): These are the primary fighters in the immune system, with various types specializing in different tasks.
- Antibodies: Proteins produced by the immune system that bind to specific targets (antigens) on foreign invaders, marking them for destruction.
- Antigens: Substances that trigger an immune response, usually found on the surface of foreign invaders.
In a healthy individual, the immune system meticulously distinguishes between "self" (the body's own cells and tissues) and "non-self" (foreign invaders). However, in autoimmune diseases, this crucial distinction breaks down. The immune system loses its tolerance for self-antigens, triggering an attack on the body's own tissues. This leads to inflammation, tissue damage, and a variety of symptoms.
The Mechanisms Behind Autoimmune Diseases
The exact mechanisms that trigger autoimmunity are not fully understood, but several factors are believed to play a role:
- Genetic predisposition: Certain genes increase the risk of developing autoimmune diseases. However, having these genes doesn't guarantee that someone will develop a condition.
- Environmental triggers: Factors like infections, exposure to toxins, or certain medications can trigger an autoimmune response in susceptible individuals.
- Hormonal influences: Autoimmune diseases are more common in women than men, suggesting a role for hormones in their development.
- Epigenetic factors: Changes in gene expression that are not due to changes in the DNA sequence itself can also contribute.
The process of autoimmunity often involves several steps:
- Loss of tolerance: The immune system loses its ability to distinguish between self and non-self.
- Activation of autoreactive cells: Immune cells that target self-antigens become activated.
- Inflammation and tissue damage: The activated immune cells attack the body's own tissues, causing inflammation and damage.
- Organ dysfunction: The damage to tissues and organs can lead to impaired function and various symptoms.
Examples of Autoimmune Diseases
Now let's examine several scenarios to determine if they describe an autoimmune disease:
Scenario 1: A patient experiences persistent joint pain and swelling, along with fatigue and low-grade fever. Blood tests reveal elevated levels of rheumatoid factor and anti-cyclic citrullinated peptide (CCP) antibodies.
Analysis: This scenario strongly suggests rheumatoid arthritis (RA), a classic autoimmune disease. RA is characterized by inflammation of the joints, leading to pain, swelling, and stiffness. The presence of rheumatoid factor and anti-CCP antibodies, which are markers of autoimmunity, confirms the diagnosis. The immune system attacks the synovium (the lining of the joints), causing chronic inflammation and damage.
Scenario 2: A patient develops a skin rash characterized by red, scaly patches. The rash is itchy and painful, and it worsens with sun exposure. A biopsy reveals inflammation of the skin and infiltration of immune cells.
Analysis: This description is consistent with psoriasis, a common autoimmune skin disease. While the exact autoimmune mechanism isn't fully understood, it involves the immune system attacking skin cells, leading to rapid skin cell growth and the characteristic scaly plaques. The inflammation and immune cell infiltration in the biopsy further support an autoimmune etiology.
Scenario 3: A patient presents with increasing muscle weakness and fatigue, particularly affecting the muscles of the eyes and throat. Blood tests show elevated levels of muscle enzymes, and an electromyogram (EMG) shows abnormal muscle activity.
Analysis: This scenario might indicate myasthenia gravis (MG), another autoimmune disease. In MG, the immune system attacks the receptors at the neuromuscular junction, impairing the communication between nerves and muscles. This leads to muscle weakness and fatigue that worsen with activity.
Scenario 4: A patient experiences frequent urination, increased thirst, and unexplained weight loss. Blood tests reveal high blood sugar levels (hyperglycemia).
Analysis: While this scenario points to diabetes, it doesn't automatically indicate an autoimmune disease. Type 1 diabetes is an autoimmune condition where the immune system destroys the insulin-producing cells in the pancreas. However, Type 2 diabetes is largely related to insulin resistance and not directly caused by autoimmunity. Further investigation, including antibody testing, would be needed to determine if the diabetes is of the autoimmune type.
Scenario 5: A patient experiences recurrent episodes of inflammation in the intestines, characterized by abdominal pain, diarrhea, and weight loss. A colonoscopy reveals ulcerations and inflammation of the intestinal lining.
Analysis: This description could be consistent with inflammatory bowel disease (IBD), encompassing conditions like Crohn's disease and ulcerative colitis. IBD is believed to have an autoimmune component, although the exact mechanisms are still unclear. The immune system attacks the intestinal lining, causing chronic inflammation and damage.
Scenario 6: A patient develops a butterfly-shaped rash across their face, along with joint pain, fatigue, and fever. Blood tests reveal elevated levels of antinuclear antibodies (ANAs).
Analysis: This scenario strongly suggests systemic lupus erythematosus (SLE), a systemic autoimmune disease. SLE is characterized by inflammation in multiple organs and tissues. The characteristic rash, joint pain, and elevated ANA levels are all indicators of this autoimmune disorder. The immune system attacks various components of the body, including DNA, causing a wide range of symptoms.
Scenario 7: A patient experiences numbness and tingling in their extremities, along with muscle weakness and balance problems. An MRI of the brain shows lesions consistent with demyelination.
Analysis: This scenario is consistent with multiple sclerosis (MS), a chronic autoimmune disease affecting the central nervous system. In MS, the immune system attacks the myelin sheath that protects nerve fibers, leading to demyelination and impaired nerve conduction. This causes a wide range of neurological symptoms.
Diagnosing Autoimmune Diseases
Diagnosing autoimmune diseases can be challenging, as symptoms can be varied and often mimic other conditions. Diagnosis typically involves:
- Medical history and physical examination: Doctors gather information about symptoms and conduct a thorough physical exam.
- Blood tests: These tests can detect antibodies that are characteristic of certain autoimmune diseases.
- Imaging tests: Such as X-rays, ultrasounds, CT scans, or MRIs, can help visualize affected organs and tissues.
- Biopsies: A small tissue sample is taken for microscopic examination to assess inflammation and immune cell infiltration.
Managing Autoimmune Diseases
There's no cure for most autoimmune diseases, but treatments aim to manage symptoms and prevent disease progression. These treatments often include:
- Medications: Such as corticosteroids to reduce inflammation, immunosuppressants to dampen the immune response, and disease-modifying antirheumatic drugs (DMARDs) for conditions like RA.
- Lifestyle changes: Including diet, exercise, and stress management techniques, can play a significant role in managing symptoms.
- Physical therapy and occupational therapy: Can help improve physical function and quality of life.
Conclusion
Autoimmune diseases are complex disorders characterized by the immune system's attack on the body's own tissues. Understanding the underlying mechanisms and recognizing the various clinical presentations are crucial for accurate diagnosis and effective management. This article has highlighted several scenarios and demonstrated how to identify potential autoimmune disorders based on clinical symptoms and laboratory findings. Early diagnosis and appropriate management are vital in minimizing the impact of these diseases and improving patients' quality of life. It's always important to consult with a healthcare professional for accurate diagnosis and tailored treatment plans for any health concerns.
Latest Posts
Latest Posts
-
Artworks Made Using Alternative Media And Processes
Mar 22, 2025
-
A Picture Composed Of Straight And Curved Lines
Mar 22, 2025
-
A Nurse Is Evaluating A Clients Use Of A Cane
Mar 22, 2025
-
How Much Does A Premium Delivery Experience Affect Cx Scores
Mar 22, 2025
-
You Want To Place A Piece Of Glass Tubing
Mar 22, 2025
Related Post
Thank you for visiting our website which covers about Which Of The Following Examples Below Describes An Autoimmune Disease . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
