Why Would An Enlarged Prostate Interfere With Urination Quizlet
Breaking News Today
Mar 17, 2025 · 6 min read
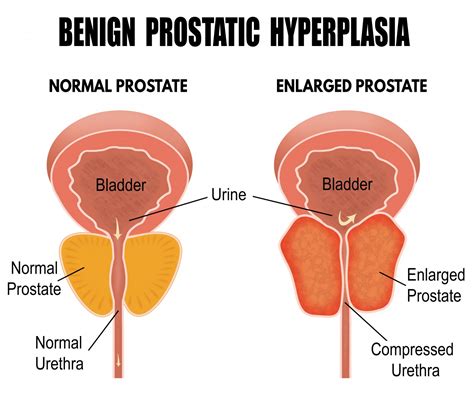
Table of Contents
Why Would an Enlarged Prostate Interfere With Urination? A Comprehensive Guide
An enlarged prostate, also known as benign prostatic hyperplasia (BPH), is a common condition affecting men as they age. It's characterized by the growth of the prostate gland, which surrounds the urethra, the tube that carries urine from the bladder. This enlargement can significantly interfere with urination, leading to a range of bothersome and sometimes serious symptoms. This article delves into the reasons why an enlarged prostate impacts urination, exploring the anatomy, physiology, and consequences of this prevalent condition.
Understanding the Anatomy and Physiology
To understand why BPH interferes with urination, it's crucial to grasp the anatomy of the urinary system and the role of the prostate gland. The prostate, a walnut-sized gland located below the bladder, plays a vital role in male reproductive health by producing seminal fluid. However, its location is key to understanding BPH's impact on urination.
The Urethra's Crucial Role
The urethra passes through the center of the prostate. As the prostate enlarges, it compresses the urethra, narrowing its passage and hindering the flow of urine. This compression is the primary reason why men with BPH experience urinary problems. Imagine trying to squeeze toothpaste out of a tube that's almost completely closed – that's essentially what's happening to the urethra in BPH.
The Bladder's Response to Obstruction
The bladder, tasked with storing urine, also plays a crucial role in the symptoms of BPH. As the flow of urine is obstructed by the enlarged prostate, the bladder must work harder to empty itself. This increased effort can lead to several consequences:
- Increased bladder pressure: The bladder needs to generate more pressure to overcome the obstruction, potentially leading to bladder wall thickening and weakening over time.
- Incomplete bladder emptying: The narrowed urethra may prevent the complete emptying of the bladder, leaving residual urine behind. This residual urine increases the risk of urinary tract infections (UTIs).
- Bladder muscle overactivity: The bladder's muscles may become overactive in an attempt to overcome the obstruction, leading to frequent and urgent urination.
The Mechanisms of Urinary Interference in BPH
Several mechanisms contribute to the urinary problems experienced by men with BPH:
1. Urethral Compression and Obstruction:
This is the most significant factor. The enlarged prostate physically squeezes the urethra, reducing its diameter and restricting urine flow. The severity of the obstruction directly correlates with the size of the prostate and the degree of urethral compression. This can range from mild discomfort to complete urinary retention, requiring immediate medical attention.
2. Changes in Bladder Function:
As mentioned, the bladder adapts to the obstruction by increasing pressure and contracting more forcefully. However, this compensatory mechanism can eventually lead to bladder dysfunction, including:
- Detrusor Instability: This refers to involuntary bladder contractions, resulting in urinary urgency and frequency. It's a common symptom of BPH and can significantly impact a man's quality of life.
- Reduced Bladder Compliance: The bladder's ability to expand and store urine diminishes, resulting in increased frequency and urgency. This is often accompanied by a feeling of incomplete emptying, even after urination.
3. Changes in Urine Flow Dynamics:
The obstruction caused by the enlarged prostate affects the dynamics of urine flow. This can manifest as:
- Weak urinary stream: The urine stream becomes slow, weak, and interrupted. This is a classic symptom of BPH, and many men initially notice this as their primary concern.
- Hesitancy: Men with BPH often experience difficulty initiating urination, needing to strain or wait for the stream to start.
- Straining during urination: Increased effort is required to empty the bladder, which can place additional strain on the heart and other bodily systems.
- Post-void dribbling: After urination, urine may continue to drip from the urethra due to incomplete bladder emptying.
4. Increased Risk of Urinary Tract Infections (UTIs):
The residual urine left behind in the bladder after urination provides an ideal breeding ground for bacteria, significantly increasing the risk of UTIs. This is particularly true in men with severely enlarged prostates. UTIs can cause pain, discomfort, and fever, and if left untreated, can lead to more serious complications.
Specific Symptoms and Their Relationship to Prostate Enlargement
The symptoms of BPH are highly variable, depending on the degree of prostate enlargement and the individual's response. Some common symptoms directly linked to the interference with urination include:
- Frequency: Needing to urinate more often than usual, particularly at night (nocturia).
- Urgency: A sudden, compelling urge to urinate that's difficult to control.
- Nocturia: Waking up multiple times during the night to urinate.
- Hesitancy: Difficulty starting the urine stream.
- Weak stream: A reduced force and flow of urine.
- Intermittency: A stopping and starting urine stream.
- Straining to urinate: Having to push hard to empty the bladder.
- Incomplete emptying: Feeling like the bladder hasn't fully emptied even after urination.
- Post-void dribbling: Leaking urine after urination.
Diagnostic Tests and Assessment
Diagnosis of BPH typically involves a physical examination, including a digital rectal exam (DRE) to assess the size and consistency of the prostate. Additional tests might include:
- Urinalysis: To rule out urinary tract infections.
- Blood tests: To assess kidney function and rule out other potential causes of urinary symptoms.
- Uroflowmetry: Measures the rate and volume of urine flow, helping to quantify the severity of obstruction.
- Post-void residual (PVR) measurement: Uses ultrasound or catheterization to determine the amount of urine remaining in the bladder after urination, indicating incomplete emptying.
Treatment Options for BPH
Treatment options for BPH range from watchful waiting (monitoring symptoms without active intervention) to medication and surgery, depending on the severity of symptoms and the patient's overall health.
Medication:
Several medications are effective in managing BPH symptoms, including:
- Alpha-blockers: Relax the muscles in the prostate and bladder neck, improving urine flow.
- 5-alpha-reductase inhibitors: Reduce the size of the prostate gland over time.
- Combination therapy: Often used to combine the benefits of alpha-blockers and 5-alpha-reductase inhibitors.
Minimally Invasive Procedures:
These procedures offer less invasive alternatives to surgery:
- Transurethral microwave thermotherapy (TUMT): Uses heat to destroy prostate tissue.
- Transurethral needle ablation (TUNA): Uses heat to destroy prostate tissue.
- Laser therapy: Uses laser energy to destroy prostate tissue.
Surgery:
Surgery may be necessary in cases of severe BPH or complications such as urinary retention:
- Transurethral resection of the prostate (TURP): A common surgical procedure that removes excess prostate tissue.
- Open prostatectomy: Involves a larger surgical incision to remove prostate tissue.
Conclusion: Living with BPH
An enlarged prostate's interference with urination significantly impacts a man's quality of life. The various mechanisms by which BPH affects urination underscore the importance of seeking medical attention if you experience bothersome symptoms. Early diagnosis and appropriate management are key to mitigating the impact of BPH and maintaining urinary health. Remember, this information is for educational purposes only and should not replace professional medical advice. Consult your doctor to discuss your symptoms and determine the best course of treatment tailored to your specific needs. Open communication with your healthcare provider is crucial for effective management and a better quality of life.
Latest Posts
Latest Posts
-
Treatment That Includes A Focus On Personal Strengths And Development
Mar 18, 2025
-
Which Is Not A Form Of Maltreatment
Mar 18, 2025
-
If An Individual Is Heterozygous For A Particular Trait
Mar 18, 2025
-
If You Add More Enzyme The Reaction Will
Mar 18, 2025
-
The Purpose Of A Hazcom Program Is To Ensure That
Mar 18, 2025
Related Post
Thank you for visiting our website which covers about Why Would An Enlarged Prostate Interfere With Urination Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
