A Patient With Copd On Positive Pressure Ventilation Quizlet
Breaking News Today
Mar 31, 2025 · 7 min read
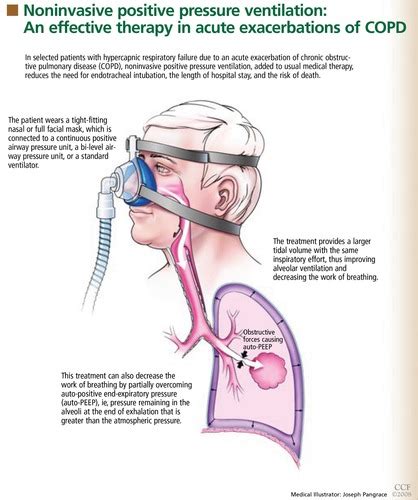
Table of Contents
A Patient with COPD on Positive Pressure Ventilation: A Comprehensive Guide
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease characterized by airflow limitation that's not fully reversible. Patients with severe COPD often require positive pressure ventilation (PPV) to support their breathing. Understanding the complexities of managing a COPD patient on PPV is crucial for healthcare professionals. This in-depth guide explores various aspects of this challenging clinical scenario, addressing key considerations for assessment, management, and potential complications.
Understanding COPD and the Rationale for Positive Pressure Ventilation
COPD encompasses conditions like emphysema and chronic bronchitis, both resulting in significant airflow obstruction. This obstruction makes it difficult to exhale completely, leading to air trapping in the lungs and hyperinflation. Over time, this puts a strain on the respiratory muscles, leading to respiratory failure.
Positive pressure ventilation (PPV), also known as mechanical ventilation, involves delivering breaths to the patient using positive pressure to inflate the lungs. This is fundamentally different from negative pressure ventilation, where the patient's own respiratory effort expands the chest cavity. PPV is used in COPD patients when their respiratory muscles are too weak to maintain adequate oxygenation and ventilation, or when their respiratory drive is compromised.
Indications for PPV in COPD Patients
Several factors can necessitate PPV in a COPD patient:
- Acute Exacerbation of COPD (AECOPD): AECOPD is characterized by a worsening of respiratory symptoms, often requiring hospitalization and potentially PPV.
- Respiratory Failure: This occurs when the lungs cannot adequately oxygenate the blood or remove carbon dioxide (CO2). PPV is critical in supporting gas exchange in these situations.
- Severe Hypercapnia: Elevated carbon dioxide levels (hypercapnia) can lead to respiratory acidosis and further compromise the patient's condition, necessitating PPV.
- Respiratory Muscle Fatigue: Prolonged respiratory effort during an exacerbation can lead to muscle fatigue, resulting in the inability to sustain adequate ventilation.
- Impaired Consciousness: Reduced levels of consciousness may hinder the patient's ability to effectively ventilate. PPV helps ensure adequate gas exchange.
Assessment and Monitoring of COPD Patients on PPV
Effective management of a COPD patient on PPV requires meticulous assessment and ongoing monitoring. The following parameters are crucial:
1. Respiratory Assessment:
- Respiratory Rate and Pattern: Observe for tachypnea (rapid breathing), bradypnea (slow breathing), use of accessory muscles, and any abnormal breathing patterns.
- Breath Sounds: Auscultate lung fields for wheezes, rhonchi, crackles, or diminished breath sounds, indicating airway obstruction or fluid accumulation.
- Oxygen Saturation (SpO2): Continuous monitoring of SpO2 using pulse oximetry is essential to ensure adequate oxygenation.
- End-Tidal Carbon Dioxide (EtCO2): Monitoring EtCO2 provides real-time information on CO2 elimination and ventilation effectiveness.
- Arterial Blood Gases (ABGs): ABGs provide a detailed assessment of blood oxygen and carbon dioxide levels, pH, and bicarbonate, allowing for precise adjustments to ventilation settings.
2. Cardiovascular Assessment:
- Heart Rate and Rhythm: Monitor for tachycardia (rapid heart rate) or arrhythmias, which can be related to hypoxia or the effects of medications.
- Blood Pressure: Assess for hypotension or hypertension, which may be associated with respiratory compromise or fluid imbalances.
3. Neurological Assessment:
- Level of Consciousness: Assess the patient's alertness and orientation, noting any changes.
- Mental Status: Evaluate for confusion, lethargy, or other cognitive impairments.
4. Other Important Assessments:
- Fluid Balance: Closely monitor fluid intake and output to prevent fluid overload or dehydration.
- Electrolyte Levels: Assess for electrolyte imbalances, particularly potassium, which can be affected by diuretics or other medications.
- Sedation Level: Monitor sedation level if sedation is required, and adjust accordingly.
Ventilator Settings and Management Strategies
The ventilator settings for a COPD patient require careful individualization based on their specific clinical condition and response to therapy. Here are some key considerations:
1. Ventilation Modes:
- Volume-Controlled Ventilation (VCV): This mode delivers a preset tidal volume (VT) at a set respiratory rate (RR). It's often used initially for patients with severe respiratory distress to ensure adequate ventilation.
- Pressure-Controlled Ventilation (PCV): This mode delivers a preset pressure for a set inspiratory time. It's often preferred for patients with COPD due to its ability to minimize airway pressures and barotrauma.
- Pressure Support Ventilation (PSV): This mode provides pressure support to each patient-initiated breath, assisting the patient's spontaneous breathing effort. It's often used during weaning from mechanical ventilation.
- Synchronized Intermittent Mandatory Ventilation (SIMV): This mode combines mandatory breaths with spontaneous breaths, allowing the patient to participate actively in breathing while receiving assistance when needed.
2. Key Ventilator Parameters:
- Tidal Volume (VT): The volume of air delivered with each breath. In COPD, lower VT is often preferred to minimize barotrauma and air trapping.
- Respiratory Rate (RR): The number of breaths delivered per minute. The RR should be adjusted based on the patient's blood gas levels and respiratory effort.
- Positive End-Expiratory Pressure (PEEP): The pressure maintained in the airways at the end of exhalation. PEEP helps keep the alveoli open and improve oxygenation. It must be carefully titrated in COPD patients to avoid excessive air trapping.
- Inspiratory Time (I-time): The duration of inspiration. Longer I-time can be beneficial for patients with severe airflow obstruction.
- Fraction of Inspired Oxygen (FiO2): The concentration of oxygen in the inspired gas. FiO2 should be adjusted to maintain adequate oxygen saturation while minimizing oxygen toxicity.
3. Weaning from Mechanical Ventilation:
Weaning from PPV is a gradual process that should be initiated when the patient meets specific criteria:
- Improved Gas Exchange: Adequate oxygenation and CO2 removal without excessive ventilator support.
- Improved Respiratory Muscle Strength: Ability to maintain adequate breathing effort without ventilator assistance.
- Hemodynamic Stability: Stable blood pressure and heart rate.
- Absence of Serious Complications: Resolution or stable management of any co-morbid conditions.
Weaning strategies can include reducing ventilator support gradually, using spontaneous breathing trials, or employing non-invasive ventilation techniques.
Potential Complications of PPV in COPD Patients
PPV, while life-saving, carries potential complications:
- Barotrauma: High airway pressures can cause damage to the lungs, leading to pneumothorax, pneumomediastinum, or subcutaneous emphysema.
- Volutrauma: Excessive tidal volumes can injure the lung tissue.
- Atelectasis: Collapse of alveoli due to inadequate ventilation.
- Ventilator-Associated Pneumonia (VAP): Infection acquired during mechanical ventilation.
- Acute Kidney Injury (AKI): Fluid overload or nephrotoxic medications can contribute to AKI.
- Cardiac Arrhythmias: Electrolyte imbalances or hypoxia can trigger cardiac arrhythmias.
- Gastrointestinal Bleeding: Stress ulcers are common in critically ill patients on PPV.
Careful monitoring and proactive management of these complications are crucial to ensure optimal patient outcomes.
Role of Non-Invasive Ventilation (NIV)
Non-invasive ventilation (NIV) techniques, such as continuous positive airway pressure (CPAP) and bilevel positive airway pressure (BiPAP), offer an alternative to invasive PPV. NIV can be used in selected COPD patients to improve ventilation and oxygenation, delaying or avoiding the need for intubation and invasive PPV. However, NIV is not suitable for all COPD patients, and careful assessment is necessary to determine its appropriateness.
Pharmacologic Management
Pharmacologic therapy plays a crucial role in managing COPD patients on PPV:
- Bronchodilators: Beta-agonists (e.g., albuterol) and anticholinergics (e.g., ipratropium) help relax airway smooth muscles and improve airflow.
- Corticosteroids: Reduce airway inflammation and improve lung function. Systemic or inhaled corticosteroids may be used.
- Antibiotics: Treat bacterial infections that may contribute to AECOPD.
- Sedatives and Analgesics: May be necessary to reduce anxiety and pain, particularly during initial stages of mechanical ventilation.
- Diuretics: Can help manage fluid overload.
Psychological and Social Support
COPD is a chronic and debilitating disease, and PPV can be a stressful experience for both the patient and their family. Providing adequate psychological and social support is crucial to improve patient compliance, reduce anxiety, and enhance the overall recovery process. This includes involving family members in care decisions, providing education about the disease and treatment, and offering access to psychosocial resources.
Conclusion
Managing a COPD patient on positive pressure ventilation requires a comprehensive approach involving meticulous assessment, careful ventilator management, proactive monitoring for complications, and integrated pharmacologic and supportive care. Understanding the physiological complexities of COPD, the rationale for PPV, and potential complications is paramount for healthcare professionals involved in the care of these patients. Through a multidisciplinary team approach, encompassing respiratory therapists, physicians, nurses, and other healthcare professionals, optimal outcomes can be achieved, improving the quality of life for patients with COPD who require mechanical ventilation. Remember, this information is for educational purposes and should not be considered medical advice. Always consult with a qualified healthcare professional for diagnosis and treatment of any medical condition.
Latest Posts
Latest Posts
-
The Greek Words Demos And Kratis Together Mean
Apr 02, 2025
-
Essentials Of Radiographic Physics And Imaging Chapter 1
Apr 02, 2025
-
A Patients Refusal Of Ems Treatment Must Be
Apr 02, 2025
-
In The Hospitality Industry The Concept Of Perishability Means
Apr 02, 2025
-
Where Do Broadside Collisions Most Commonly Occur
Apr 02, 2025
Related Post
Thank you for visiting our website which covers about A Patient With Copd On Positive Pressure Ventilation Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
