Ace Inhibitor Medications Lower Blood Pressure By Quizlet
Breaking News Today
Mar 18, 2025 · 6 min read
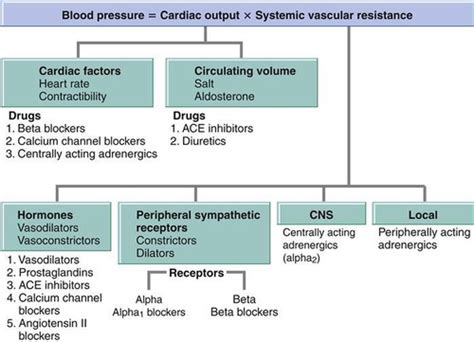
Table of Contents
ACE Inhibitor Medications: Lowering Blood Pressure Explained
ACE inhibitors are a cornerstone of blood pressure management, a class of medications prescribed globally to treat hypertension and other cardiovascular conditions. Understanding how they work, their benefits, potential side effects, and when they're prescribed is crucial for patients and healthcare professionals alike. This in-depth article explores ACE inhibitors, specifically addressing their mechanism of action in lowering blood pressure, answering common questions, and debunking misconceptions.
Understanding the Renin-Angiotensin-Aldosterone System (RAAS)
To grasp how ACE inhibitors work, it's essential to understand the renin-angiotensin-aldosterone system (RAAS). This complex hormonal system plays a vital role in regulating blood pressure and fluid balance within the body.
The RAAS Cascade: A Step-by-Step Breakdown
- Renin Release: When blood pressure drops or sodium levels decrease, the kidneys release renin, an enzyme.
- Angiotensinogen Conversion: Renin converts angiotensinogen (a liver-produced protein) into angiotensin I.
- ACE's Role: Angiotensin-converting enzyme (ACE) then converts angiotensin I into angiotensin II, a potent vasoconstrictor.
- Vasoconstriction and Aldosterone Release: Angiotensin II causes blood vessels to narrow (vasoconstriction), increasing blood pressure. It also stimulates the adrenal glands to release aldosterone.
- Aldosterone's Effect: Aldosterone promotes sodium and water retention by the kidneys, further increasing blood volume and blood pressure.
How ACE Inhibitors Work: Blocking the Cascade
ACE inhibitors work by specifically blocking the action of ACE. By inhibiting ACE, they prevent the conversion of angiotensin I to angiotensin II. This interruption significantly impacts the RAAS, leading to several beneficial effects:
Key Mechanisms of Blood Pressure Reduction:
- Reduced Vasoconstriction: The decrease in angiotensin II levels leads to less vasoconstriction, resulting in relaxed and dilated blood vessels. This allows for easier blood flow, reducing the pressure against artery walls.
- Decreased Aldosterone Release: With less angiotensin II, the adrenal glands release less aldosterone. This reduces sodium and water retention, lowering blood volume and consequently, blood pressure.
- Increased Bradykinin Levels: ACE also breaks down bradykinin, a vasodilator. ACE inhibitors increase bradykinin levels, contributing to further vasodilation and blood pressure reduction. This vasodilatory effect contributes significantly to their efficacy, especially in certain patient populations.
Benefits Beyond Blood Pressure Control
While primarily known for lowering blood pressure, ACE inhibitors offer additional cardiovascular benefits:
Protecting the Heart and Kidneys:
- Heart Protection: By reducing afterload (the pressure the heart has to pump against), ACE inhibitors ease the workload on the heart, improving its function and reducing the risk of heart failure. They're particularly beneficial for individuals with heart failure or a history of myocardial infarction (heart attack).
- Kidney Protection: ACE inhibitors are often used to protect the kidneys in conditions like diabetic nephropathy (kidney damage caused by diabetes) and chronic kidney disease. By reducing pressure within the glomeruli (filtering units of the kidneys), they help slow down kidney damage progression.
- Stroke Prevention: Lowering blood pressure and reducing afterload can help prevent strokes by improving blood flow to the brain. This is particularly important for individuals with hypertension and other risk factors for stroke.
Common ACE Inhibitors: A Quick Overview
Numerous ACE inhibitors are available, each with slight variations in their properties and potential side effects. Some commonly prescribed ACE inhibitors include:
- Lisinopril: Often a first-line choice due to its effectiveness and relatively mild side effects.
- Ramipril: Another widely used ACE inhibitor, known for its longer duration of action.
- Enalapril: A frequently prescribed ACE inhibitor, particularly for patients with heart failure.
- Captopril: Often used in initial stages of treatment or in specific patient populations due to its rapid onset of action.
Note: This list is not exhaustive, and the choice of specific medication will depend on individual factors and the patient's overall health status. Always consult a healthcare professional for guidance on medication selection.
Potential Side Effects: Understanding the Risks
While generally safe and effective, ACE inhibitors can cause some side effects. The most common include:
- Dry Cough: This is a frequent side effect, often attributed to the buildup of bradykinin. If a dry cough develops, alternative medications might be considered.
- Dizziness and Lightheadedness: These can occur, especially at the beginning of treatment, as the body adjusts to the medication's effects.
- Hyperkalemia: Increased potassium levels in the blood are a potential side effect, especially in patients with kidney problems or those taking other medications that affect potassium levels. Regular blood tests are essential to monitor potassium levels.
- Angioedema: A rare but serious side effect involving swelling of the face, lips, tongue, or throat. Immediate medical attention is required if this occurs.
Important Considerations: The severity and frequency of side effects vary significantly among individuals. Consulting with a healthcare professional is crucial to discuss any concerns or potential side effects.
When Are ACE Inhibitors Prescribed?
ACE inhibitors are widely prescribed for a range of conditions:
- Hypertension (High Blood Pressure): A primary use, often as first-line therapy, especially in patients with additional risk factors like diabetes or heart disease.
- Heart Failure: ACE inhibitors are a crucial part of heart failure management, improving symptoms and reducing mortality risk.
- Diabetic Nephropathy: Protecting the kidneys in individuals with diabetes is a vital use of ACE inhibitors.
- Post-Myocardial Infarction (Heart Attack): Reducing mortality risk and improving heart function after a heart attack.
- Chronic Kidney Disease: Slowing down the progression of chronic kidney disease and protecting kidney function.
ACE Inhibitors and Pregnancy: A Special Note
ACE inhibitors should generally be avoided during pregnancy, particularly in the second and third trimesters. They can cause serious harm to the developing fetus. Alternative blood pressure medications are usually recommended for pregnant women.
ACE Inhibitors vs. Other Blood Pressure Medications: A Comparison
ACE inhibitors are not the only class of blood pressure medications. Other options include:
- Angiotensin Receptor Blockers (ARBs): Similar to ACE inhibitors, ARBs block the effects of angiotensin II but through a different mechanism. They are sometimes used as an alternative for patients who experience a dry cough with ACE inhibitors.
- Beta-Blockers: Reduce heart rate and blood pressure, particularly beneficial for individuals with certain heart conditions.
- Calcium Channel Blockers: Relax blood vessels and lower blood pressure.
- Diuretics: Increase urine production, reducing blood volume and blood pressure.
The choice of blood pressure medication depends on various factors, including the patient's overall health, other medical conditions, and individual responses to different medications. A healthcare professional should determine the most appropriate treatment plan.
Monitoring and Management: Working with Your Doctor
Regular monitoring is crucial when taking ACE inhibitors. This includes:
- Blood Pressure Monitoring: Regular blood pressure checks help assess the effectiveness of the medication and adjust the dosage as needed.
- Kidney Function Tests: Monitoring kidney function is particularly important to detect any potential adverse effects on the kidneys.
- Potassium Levels: Regular blood tests are necessary to monitor potassium levels, especially in patients at risk of hyperkalemia.
Regular communication with your doctor is essential to discuss any side effects, concerns, or changes in your health status. Working collaboratively with your healthcare provider ensures optimal management of your blood pressure and overall cardiovascular health.
Conclusion: A Vital Role in Cardiovascular Health
ACE inhibitors have played and continue to play a pivotal role in managing hypertension and other cardiovascular diseases. Their mechanism of action, targeting the RAAS, allows for effective blood pressure control, offering significant benefits beyond simply lowering blood pressure. Understanding how they work, potential side effects, and the importance of ongoing monitoring empowers patients and healthcare providers to make informed decisions about their cardiovascular health. Always consult a healthcare professional for personalized advice and treatment. This information is for educational purposes only and should not be considered medical advice.
Latest Posts
Latest Posts
-
High Levels Of Cholesterol Can First Lead Directly To
Mar 18, 2025
-
True Or False Professional And Technical Communication Is Research Oriented
Mar 18, 2025
-
Which Best Describes The Terrorist Planning Cycle
Mar 18, 2025
-
Cdl Combination Test Questions And Answers Pdf
Mar 18, 2025
-
Life Insurance Exam Questions And Answers Pdf
Mar 18, 2025
Related Post
Thank you for visiting our website which covers about Ace Inhibitor Medications Lower Blood Pressure By Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
