Adh Causes The Reabsorption Of ________ In The Kidney Tubule.
Breaking News Today
Mar 16, 2025 · 6 min read
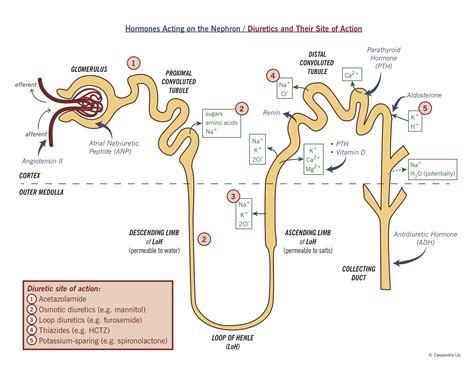
Table of Contents
ADH Causes the Reabsorption of Water in the Kidney Tubule: A Deep Dive into Antidiuretic Hormone
Antidiuretic hormone (ADH), also known as vasopressin, plays a crucial role in maintaining fluid balance within the body. Its primary function centers around regulating water reabsorption in the kidney tubules. Understanding how ADH achieves this is fundamental to grasping the intricacies of renal physiology and overall homeostasis. This article will delve deep into the mechanisms by which ADH causes the reabsorption of water in the kidney tubules, exploring its physiological impact and the consequences of dysfunction.
The Renin-Angiotensin-Aldosterone System (RAAS) and ADH: A Coordinated Effort
Before focusing solely on ADH, it's crucial to acknowledge its interaction with other hormonal systems, particularly the RAAS. The RAAS is a complex cascade that primarily regulates blood pressure and sodium balance. While ADH primarily focuses on water balance, its actions are often intertwined with the RAAS, ensuring a coordinated response to changes in fluid and electrolyte levels. For instance, low blood volume or pressure triggers the RAAS, leading to aldosterone release, which increases sodium reabsorption in the distal tubules and collecting ducts. This sodium reabsorption creates an osmotic gradient, indirectly facilitating water reabsorption, an effect further amplified by ADH. The interplay between ADH and the RAAS underscores the body's sophisticated mechanisms for maintaining homeostasis.
The Anatomy of the Nephron and ADH's Target Site
To understand ADH's mechanism of action, we must first examine the nephron, the functional unit of the kidney. The nephron consists of several distinct segments: the glomerulus, Bowman's capsule, proximal convoluted tubule (PCT), loop of Henle, distal convoluted tubule (DCT), and collecting duct. ADH primarily targets the collecting ducts, although some effects may be observed in the distal convoluted tubules. The collecting ducts are crucial for fine-tuning water reabsorption, allowing the kidneys to adjust urine concentration precisely to maintain body fluid balance.
The Collecting Duct: A Key Player in Water Balance
The collecting duct's structure is uniquely suited for its role in water reabsorption. Its cells possess specialized aquaporins, water channels embedded in their membranes. These aquaporins are not always present; their expression is tightly regulated by ADH. In the absence of ADH, the collecting duct is relatively impermeable to water, resulting in the excretion of a large volume of dilute urine.
ADH's Mechanism of Action: A Molecular Perspective
ADH, released from the posterior pituitary gland in response to increased plasma osmolality (concentration of solutes in the blood) or decreased blood volume, initiates a cascade of events leading to increased water reabsorption. Here's a step-by-step breakdown:
-
ADH Binding to V2 Receptors: ADH binds to V2 receptors located on the basolateral membranes (the side facing the interstitial fluid) of principal cells in the collecting ducts. These V2 receptors are G protein-coupled receptors, initiating a signaling cascade within the cell.
-
cAMP Activation and Protein Kinase A: V2 receptor activation stimulates adenylyl cyclase, leading to an increase in cyclic adenosine monophosphate (cAMP). cAMP then activates protein kinase A (PKA).
-
Aquaporin-2 (AQP2) Trafficking: PKA plays a critical role in regulating the trafficking of aquaporin-2 (AQP2) water channels. PKA phosphorylation of AQP2 causes its translocation from intracellular vesicles to the apical membrane (the side facing the tubular lumen) of the principal cells. This insertion of AQP2 into the apical membrane increases the water permeability of the collecting duct epithelium.
-
Water Movement Across the Epithelium: With AQP2 channels present in the apical membrane and constitutive aquaporins (AQP3 and AQP4) already located in the basolateral membrane, water can now passively move across the collecting duct epithelium from the tubular lumen into the interstitial fluid, driven by the osmotic gradient created by the reabsorption of sodium and other solutes in other parts of the nephron.
-
Increased Water Reabsorption and Concentrated Urine: The increased water permeability facilitated by ADH leads to a significant increase in water reabsorption. This results in the production of smaller volumes of more concentrated urine.
Feedback Mechanisms: Maintaining Homeostasis
The body employs a sophisticated negative feedback loop to maintain optimal plasma osmolality and blood volume. Osmoreceptors in the hypothalamus monitor plasma osmolality. When osmolality rises (indicating dehydration), the hypothalamus signals the posterior pituitary to release ADH. Conversely, when osmolality falls (indicating overhydration), ADH release is inhibited. This delicate balance ensures that water excretion is precisely regulated to maintain fluid homeostasis. Baroreceptors, sensitive to changes in blood pressure, also play a role, triggering ADH release when blood pressure falls.
Clinical Significance of ADH Dysfunction: Consequences of Imbalance
Dysfunction in the ADH system can have significant clinical consequences. Conditions involving either overproduction or underproduction of ADH can lead to severe fluid imbalances:
Syndrome of Inappropriate Antidiuretic Hormone (SIADH): Too Much ADH
SIADH results from excessive ADH secretion, leading to increased water reabsorption and hyponatremia (low sodium levels in the blood). The excess water dilutes the sodium concentration, causing symptoms like nausea, vomiting, headache, confusion, and seizures. Severe hyponatremia can be life-threatening.
Diabetes Insipidus (DI): Too Little ADH
DI, in contrast, is characterized by insufficient ADH production or action. This leads to decreased water reabsorption and polyuria (excessive urination) and polydipsia (excessive thirst). Two main types exist: central DI, due to ADH deficiency, and nephrogenic DI, due to the kidney's inability to respond to ADH. Both types result in the excretion of large volumes of dilute urine, potentially leading to dehydration and electrolyte imbalances.
Therapeutic Interventions: Targeting ADH Pathways
Understanding the mechanisms of ADH action has led to the development of various therapeutic interventions for conditions involving ADH imbalances. For instance, drugs that antagonize ADH receptors (V2 receptor antagonists) are used to treat SIADH by reducing water reabsorption. Conversely, synthetic ADH is used to treat central DI, replacing the deficient hormone.
Conclusion: ADH – A Crucial Regulator of Fluid Balance
ADH's role in regulating water reabsorption in the kidney tubules is crucial for maintaining fluid and electrolyte balance. Its intricate mechanism of action, involving receptor binding, signaling cascades, and aquaporin trafficking, exemplifies the complexity of renal physiology. Understanding this intricate process is vital for appreciating the body's ability to maintain homeostasis and for diagnosing and treating conditions resulting from ADH dysfunction. Future research continues to explore the nuances of ADH's actions and its interactions with other regulatory systems, leading to improved diagnostics and therapies for conditions related to fluid imbalance. The interplay between ADH, the RAAS, and other hormonal systems highlights the sophisticated, coordinated efforts of the body to maintain a delicate balance, emphasizing the importance of understanding this critical physiological process. The precise regulation of water balance is essential for overall health, and disruptions in this delicate system can have significant health consequences.
Latest Posts
Latest Posts
-
Olga Lucia Es De Los Estados Unidos
Mar 16, 2025
-
Which Of The Following Is True About Emotional Abuse
Mar 16, 2025
-
A Productive Cough Fever And Chills In An 80
Mar 16, 2025
-
Mrs Shields Is Covered By Original Medicare
Mar 16, 2025
-
Both The Knee And The Temporomandibular Joints
Mar 16, 2025
Related Post
Thank you for visiting our website which covers about Adh Causes The Reabsorption Of ________ In The Kidney Tubule. . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
