Both The Knee And The Temporomandibular Joints ________.
Breaking News Today
Mar 16, 2025 · 6 min read
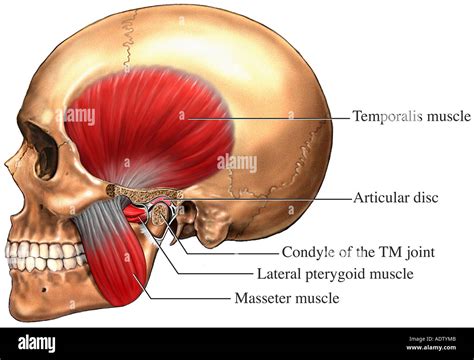
Table of Contents
Both the Knee and the Temporomandibular Joints: A Comparative Analysis of Structure, Function, and Dysfunction
The human body is a marvel of engineering, with intricate joints facilitating movement and supporting our daily activities. Among these, the knee and temporomandibular (TMJ) joints stand out due to their complexity and susceptibility to dysfunction. While seemingly disparate—one involved in locomotion, the other in speech and mastication—they share remarkable similarities in their structural components, biomechanics, and the pathologies they can experience. This article delves into a comparative analysis of the knee and TMJ, exploring their shared characteristics and unique features.
Structural Similarities and Differences
Both the knee and TMJ are classified as synovial joints, meaning they possess a synovial cavity filled with synovial fluid that lubricates the joint surfaces, reducing friction and providing nourishment to the articular cartilage. However, their specific structural components differ significantly.
The Knee Joint: A Complex Hinge
The knee, the largest joint in the human body, is a modified hinge joint allowing flexion, extension, and a small degree of medial and lateral rotation. Its structural components include:
- Femoral condyles: The rounded distal ends of the femur, articulating with the tibial plateau.
- Tibial plateau: The relatively flat superior surface of the tibia, forming the weight-bearing surface.
- Patella: The kneecap, a sesamoid bone embedded within the quadriceps tendon, increasing the mechanical advantage of the quadriceps muscle group.
- Menisci: Two C-shaped fibrocartilaginous discs (medial and lateral) that act as shock absorbers, distributing weight evenly across the joint and enhancing stability.
- Cruciate ligaments: The anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) provide crucial anteroposterior stability.
- Collateral ligaments: The medial collateral ligament (MCL) and lateral collateral ligament (LCL) provide stability against varus and valgus stresses (inward and outward forces).
- Synovial membrane: Lines the joint capsule, secreting synovial fluid.
The Temporomandibular Joint: A Unique Ginglymoarthroidal Joint
The TMJ is a unique joint, classified as a ginglymoarthroidal joint, combining characteristics of both hinge and gliding joints. It allows for a complex range of motion, including elevation, depression, protraction, retraction, and lateral excursion. Its components include:
- Mandibular condyle: The rounded projection of the mandible articulating with the temporal bone.
- Articular eminence and mandibular fossa: Structures on the temporal bone that form the articular surface.
- Articular disc: A fibrocartilaginous disc that divides the joint into two compartments: the superior and inferior joint spaces. This disc plays a critical role in distributing forces and facilitating smooth movement.
- Temporomandibular ligament: Reinforces the joint capsule, restricting excessive movement.
- Synovial membrane: Lines the joint capsule, secreting synovial fluid.
Functional Similarities and Differences
Despite their structural differences, both joints share the common function of facilitating movement. However, the type and range of motion differ significantly.
Knee Joint Function: Weight Bearing and Locomotion
The primary function of the knee is to support the body's weight and enable locomotion. Its strong ligaments and complex articular surfaces allow for weight-bearing activities, running, jumping, and other dynamic movements. The coordinated actions of muscles surrounding the knee, including the quadriceps, hamstrings, gastrocnemius, and soleus, further contribute to its functional capacity.
TMJ Function: Mastication, Speech, and Facial Expression
The TMJ's function is primarily focused on mastication (chewing), speech, and facial expressions. The coordinated actions of the masseter, temporalis, and pterygoid muscles allow for precise movements of the mandible, facilitating the efficient breakdown of food and articulation of speech. The intricate interplay of the articular disc and joint surfaces ensures smooth, coordinated movement during these functions.
Dysfunction and Pathology: A Comparative Overview
Both the knee and TMJ are prone to a variety of pathologies, many of which share similar underlying mechanisms, including trauma, overuse, and degenerative changes.
Knee Joint Pathology:
- Osteoarthritis: Degeneration of articular cartilage, leading to pain, stiffness, and reduced range of motion.
- Rheumatoid arthritis: Autoimmune disease causing inflammation and damage to the joint lining and cartilage.
- Meniscus tears: Tears in the menisci, often caused by twisting injuries, leading to pain, instability, and clicking.
- Ligament injuries (ACL, PCL, MCL, LCL): Tears or sprains of ligaments, frequently resulting from sudden twisting or direct impact.
- Patellofemoral pain syndrome: Pain around the patella, often caused by malalignment, muscle imbalances, or overuse.
TMJ Pathology:
- Temporomandibular joint disorder (TMD): An umbrella term encompassing various conditions affecting the TMJ, including pain, clicking, locking, and limited range of motion. Causes range from trauma to stress and bruxism (teeth grinding).
- Osteoarthritis: Similar to the knee, degeneration of articular cartilage leads to pain and reduced function.
- Arthritis: Other forms of arthritis, such as rheumatoid arthritis, can also affect the TMJ.
- Internal derangement: Displacement or damage to the articular disc, frequently leading to clicking, popping, or locking of the jaw.
- Myofascial pain: Muscle pain and tenderness affecting the muscles of mastication.
Shared Risk Factors and Management Strategies
Several risk factors increase the likelihood of developing dysfunction in both the knee and TMJ. These include:
- Age: Degenerative changes associated with aging are a significant risk factor for both osteoarthritis of the knee and TMJ.
- Obesity: Increased weight places additional stress on both joints, accelerating degenerative processes.
- Trauma: Direct injury or repetitive microtrauma can damage the ligaments, menisci, and articular cartilage in both the knee and TMJ.
- Genetic predisposition: A family history of joint disorders can increase the risk of developing similar problems.
- Occupational factors: Jobs involving repetitive movements or prolonged periods of kneeling or squatting may increase the risk of knee problems. Similarly, jobs demanding excessive jaw movements can increase the risk of TMJ disorders.
Management strategies for both knee and TMJ disorders share many similarities:
- Conservative management: This often involves rest, ice, compression, elevation (RICE), pain relief medications (NSAIDs), physical therapy (including range of motion exercises and strengthening), and splinting or bracing.
- Invasive procedures: In cases of severe or persistent symptoms, surgery may be necessary. For the knee, this could involve arthroscopy, meniscus repair, ligament reconstruction, or joint replacement. For the TMJ, surgical interventions may include arthroscopy, disc repositioning, or joint replacement (rare).
- Lifestyle modifications: Weight loss, improving posture, avoiding activities that aggravate symptoms, and stress management techniques are crucial components of long-term management for both knee and TMJ disorders.
Conclusion: Understanding the Connections
The knee and TMJ, despite their distinct anatomical locations and primary functions, share surprising similarities in their structure, biomechanics, and susceptibility to dysfunction. Understanding these shared characteristics can provide valuable insights into the pathophysiology, diagnosis, and management of disorders affecting both joints. While specific treatment approaches may vary, the underlying principles of conservative management, lifestyle modifications, and surgical intervention are applicable to both. Further research into the complex interplay of factors contributing to joint dysfunction in these two distinct areas could lead to more effective prevention and treatment strategies. This comparative analysis highlights the interconnectedness of the musculoskeletal system and underscores the importance of a holistic approach to managing joint-related problems.
Latest Posts
Latest Posts
-
The Revenue Recognition Principle States That Revenue
Mar 16, 2025
-
The Cognitive Behavioral Approach To Therapy Stresses
Mar 16, 2025
-
Letrs Unit 5 Session 5 Check For Understanding
Mar 16, 2025
-
This Figure Depicts The Basic Anatomy Of The
Mar 16, 2025
-
Which Is A Stroke Severity Tool That Helps Ems
Mar 16, 2025
Related Post
Thank you for visiting our website which covers about Both The Knee And The Temporomandibular Joints ________. . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
