Common Causes Of Depression In The Elderly Quizlet
Breaking News Today
Mar 17, 2025 · 7 min read
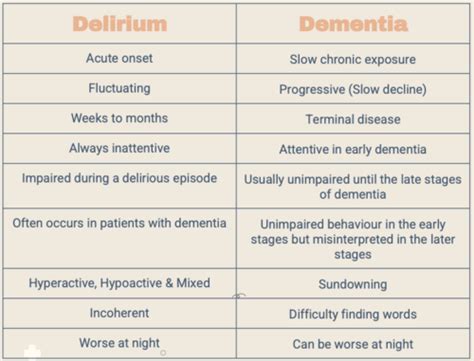
Table of Contents
Common Causes of Depression in the Elderly: A Comprehensive Guide
Depression in older adults is a significant public health concern, often underdiagnosed and undertreated. Unlike the fleeting sadness experienced by younger populations, geriatric depression can be a persistent and debilitating condition with profound impacts on physical and mental well-being. Understanding its common causes is crucial for effective prevention and intervention. This article delves into the multifaceted nature of late-life depression, exploring various contributing factors and highlighting the importance of early recognition and appropriate care.
Biological Factors: The Body's Role in Depression
The biological underpinnings of depression are complex and not fully understood, but several key factors play a significant role, particularly in older adults:
1. Neurotransmitter Imbalances:
The brain relies on a delicate balance of neurotransmitters, chemical messengers that transmit signals between nerve cells. Imbalances in serotonin, dopamine, and norepinephrine are strongly implicated in depression. Aging itself can affect the production and utilization of these neurotransmitters, increasing vulnerability. This neurochemical disruption can lead to decreased mood, loss of motivation, and cognitive difficulties, all hallmarks of depression.
2. Hormonal Changes:
Significant hormonal shifts occur with age, particularly in women after menopause. Decreased estrogen levels can contribute to mood disturbances, sleep problems, and increased anxiety—all risk factors for depression. Changes in other hormones, such as cortisol (the stress hormone), can also disrupt the brain's delicate equilibrium and contribute to depressive symptoms.
3. Chronic Medical Conditions:
The prevalence of chronic diseases increases significantly with age. Conditions like heart disease, stroke, diabetes, arthritis, and cancer can directly impact mood and increase the risk of depression. The pain, disability, and limitations associated with these conditions can lead to feelings of helplessness, isolation, and despair. Furthermore, the medications used to treat these conditions can sometimes have depression as a side effect.
4. Brain Changes:
Structural and functional changes in the brain can occur with age, impacting mood regulation and cognitive function. For example, reduced blood flow to certain brain regions, as well as changes in brain volume, can contribute to depressive symptoms. These changes are not necessarily indicative of dementia but can still significantly influence mental well-being.
Psychological Factors: The Mind's Contribution to Depression
Beyond biological factors, psychological elements play a critical role in the development and severity of depression in older adults:
1. Loss and Grief:
Older adults experience a higher frequency of significant losses than younger individuals. The loss of a spouse, close friends, family members, or pets can trigger intense grief, which can evolve into depression if not properly processed. The cumulative effect of multiple losses over time can significantly impact mental health.
2. Cognitive Changes:
Mild cognitive impairment (MCI) and dementia, while not direct causes of depression, often co-occur. The cognitive decline associated with these conditions can lead to frustration, confusion, loss of independence, and social isolation, all contributing factors to depression. The challenges of managing these conditions can further burden caregivers and individuals themselves, exacerbating depressive symptoms.
3. Stress and Trauma:
Past trauma, current stressors, and ongoing life challenges can all contribute to depression. Financial difficulties, social isolation, loneliness, and housing instability can be particularly impactful on older adults. The experience of stressful life events, such as relocation, hospitalization, or the loss of driving ability, can trigger or worsen depressive symptoms.
4. Personality Factors:
Pre-existing personality traits and coping mechanisms can influence vulnerability to depression. Individuals who are already prone to anxiety, pessimism, or have difficulty adapting to change may be at increased risk. Similarly, individuals with poor coping skills or limited social support may be less resilient to life's stressors.
Social Factors: The Impact of Environment and Relationships
Social and environmental factors are integral to understanding the complexities of late-life depression:
1. Social Isolation and Loneliness:
Social isolation and loneliness are pervasive problems among older adults and strong predictors of depression. Loss of social connections, reduced mobility, and difficulties engaging in social activities contribute to feelings of isolation, which can significantly impact mood and well-being. The lack of meaningful social interaction can exacerbate existing mental health challenges.
2. Reduced Social Support:
Adequate social support is crucial for maintaining mental well-being. A decline in social support, whether due to loss of loved ones, decreased social engagement, or strained relationships, can leave older adults feeling vulnerable and unsupported, increasing their susceptibility to depression.
3. Financial Difficulties:
Financial strain can be a significant stressor, particularly for older adults on fixed incomes. Worries about affording essential expenses, such as medication, housing, and food, can significantly impact mental health and contribute to feelings of anxiety and hopelessness, ultimately leading to depression.
4. Life Transitions and Changes:
Significant life transitions, such as retirement, relocation to a nursing home or assisted living facility, or the loss of a driving license, can trigger emotional distress and contribute to depression. Adapting to these changes can be challenging, and the associated feelings of loss of independence and control can exacerbate existing vulnerabilities.
Recognizing the Signs: Early Detection is Key
Early recognition of depression in older adults is crucial for effective intervention. However, it’s important to remember that depression in the elderly can present differently than in younger populations. Symptoms may be less obvious and can manifest as physical complaints rather than overt sadness.
Common Symptoms:
- Persistent sadness, low mood, or feelings of hopelessness.
- Loss of interest or pleasure in activities once enjoyed (anhedonia).
- Changes in appetite or weight (significant weight loss or gain).
- Sleep disturbances (insomnia or excessive sleeping).
- Fatigue or loss of energy.
- Feelings of worthlessness or excessive guilt.
- Difficulty concentrating, remembering things, or making decisions.
- Restlessness or irritability.
- Recurring thoughts of death or suicide.
- Physical complaints such as aches, pains, or digestive problems.
It is essential to consult a healthcare professional if you or a loved one is experiencing several of these symptoms. A comprehensive assessment is necessary to rule out other underlying medical conditions and to determine the most appropriate course of treatment.
Treatment and Management: A Multifaceted Approach
Effective management of depression in older adults often requires a multimodal approach, combining various interventions tailored to the individual's needs and circumstances:
- Medication: Antidepressant medications are often prescribed to address neurotransmitter imbalances. The choice of medication and dosage is carefully considered based on the individual's medical history, other medications they are taking, and potential side effects.
- Psychotherapy: Different therapeutic approaches, such as cognitive-behavioral therapy (CBT) and interpersonal therapy (IPT), can help older adults identify and challenge negative thought patterns, develop coping strategies, and improve their interpersonal relationships. These therapies are particularly helpful in addressing the psychological and social factors contributing to depression.
- Lifestyle Changes: Encouraging healthy lifestyle choices, such as regular exercise, a balanced diet, and sufficient sleep, can significantly improve mood and well-being. Engaging in enjoyable activities and pursuing hobbies can also boost morale and reduce feelings of isolation.
- Social Support: Building and maintaining strong social connections is crucial. Encouraging participation in social activities, connecting with family and friends, and joining support groups can significantly enhance mood and improve overall quality of life.
- Caregiver Support: Providing support and education to caregivers is essential. Caregiving can be physically and emotionally demanding, and caregivers may need assistance managing their own stress and burnout to effectively support their loved ones.
Conclusion: Addressing a Significant Public Health Challenge
Depression in older adults is a complex and multifaceted condition requiring a comprehensive and individualized approach. Understanding the diverse biological, psychological, and social factors that contribute to late-life depression is crucial for effective prevention and intervention. Early recognition, prompt diagnosis, and appropriate treatment are essential to improving the quality of life for older adults experiencing this debilitating condition. A collaborative effort involving healthcare professionals, family members, caregivers, and the individuals themselves is vital in addressing this significant public health challenge and promoting the mental well-being of our aging population. Further research and public awareness campaigns are essential to reduce the stigma associated with depression and to ensure that older adults receive the timely and appropriate care they need. By acknowledging the complexities of geriatric depression and implementing multifaceted interventions, we can strive to support the mental and physical well-being of our elderly population.
Latest Posts
Latest Posts
-
Which Best Describes The Terrorist Planning Cycle
Mar 18, 2025
-
Cdl Combination Test Questions And Answers Pdf
Mar 18, 2025
-
Life Insurance Exam Questions And Answers Pdf
Mar 18, 2025
-
The Direct Carry Is Used To Transfer A Patient
Mar 18, 2025
-
The Emancipation Proclamation Of January 1 1863 Quizlet
Mar 18, 2025
Related Post
Thank you for visiting our website which covers about Common Causes Of Depression In The Elderly Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
