Drugs Affecting The Respiratory System Edapt Quizlet
Breaking News Today
Mar 31, 2025 · 6 min read
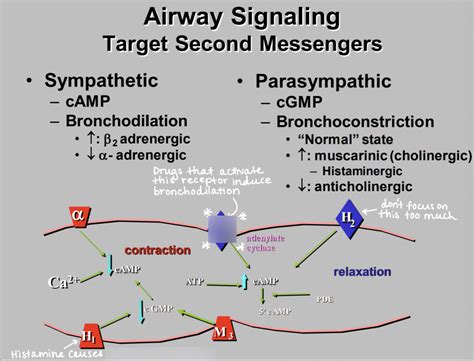
Table of Contents
Drugs Affecting the Respiratory System: A Comprehensive Guide
This comprehensive guide explores the various drugs affecting the respiratory system, delving into their mechanisms of action, therapeutic uses, adverse effects, and contraindications. We'll cover both medications used to treat respiratory conditions and those that may negatively impact respiratory function. This in-depth analysis is intended to be educational and should not be considered medical advice. Always consult with a healthcare professional before starting or changing any medication regimen.
Keywords: respiratory drugs, respiratory system, bronchodilators, anti-inflammatory drugs, mucolytics, cough suppressants, respiratory depressants, adverse effects, drug interactions, COPD, asthma, pneumonia, pulmonary embolism.
I. Bronchodilators: Opening the Airways
Bronchodilators are a cornerstone in the treatment of obstructive airway diseases like asthma and chronic obstructive pulmonary disease (COPD). They work by relaxing the smooth muscles surrounding the airways, leading to bronchodilation and improved airflow. The two main classes are:
A. Beta-2 Agonists: Stimulating the Sympathetic System
Beta-2 agonists mimic the effects of adrenaline on beta-2 receptors in the lungs. This leads to smooth muscle relaxation and bronchodilation. They are available in various forms, including:
-
Short-acting beta-2 agonists (SABAs): These provide quick relief from bronchospasm, often used for rescue medication during acute exacerbations. Examples include albuterol (salbutamol) and levalbuterol. Key features: rapid onset, short duration of action.
-
Long-acting beta-2 agonists (LABAs): These provide longer-lasting bronchodilation, typically used for maintenance therapy in conjunction with other medications. Examples include salmeterol and formoterol. Key features: slower onset, longer duration of action, not for rescue use.
Adverse effects: Tremors, tachycardia, nervousness, insomnia, and potential for paradoxical bronchospasm (in rare cases).
B. Anticholinergics: Blocking the Parasympathetic System
Anticholinergics block the action of acetylcholine, a neurotransmitter that causes bronchoconstriction. This leads to relaxation of airway smooth muscles and improved airflow. Examples include ipratropium bromide and tiotropium bromide.
-
Ipratropium bromide: Often used as a short-acting bronchodilator, either alone or in combination with a beta-2 agonist.
-
Tiotropium bromide: A long-acting anticholinergic used for maintenance therapy in COPD.
Adverse effects: Dry mouth, constipation, blurred vision, urinary retention.
II. Anti-inflammatory Drugs: Reducing Inflammation
Inflammation plays a significant role in the pathogenesis of many respiratory diseases. Anti-inflammatory drugs help reduce airway inflammation, thereby improving lung function and reducing the frequency and severity of exacerbations.
A. Corticosteroids: Powerful Anti-inflammatory Agents
Inhaled corticosteroids (ICS) are the mainstay of asthma and COPD treatment. They effectively reduce inflammation, but their effects are not immediate. Examples include fluticasone, budesonide, and beclomethasone.
Mechanism of action: Corticosteroids bind to intracellular receptors, leading to the suppression of inflammatory mediators.
Adverse effects: Oral thrush (candidiasis), hoarseness, dysphonia, increased risk of pneumonia (especially with high doses).
B. Leukotriene Modifiers: Blocking Inflammatory Pathways
Leukotrienes are potent inflammatory mediators involved in asthma pathogenesis. Leukotriene modifiers, such as montelukast and zafirlukast, block the action of leukotrienes, reducing inflammation and bronchospasm.
Mechanism of action: These drugs selectively inhibit the activity of leukotriene receptors.
Adverse effects: Headache, nausea, abdominal pain, elevated liver enzymes.
C. Mast Cell Stabilizers: Preventing Inflammatory Mediator Release
Mast cell stabilizers, such as cromolyn sodium and nedocromil sodium, prevent the release of inflammatory mediators from mast cells. They are primarily used in the prophylaxis of asthma.
Mechanism of action: These drugs stabilize mast cell membranes, preventing the release of histamine and other inflammatory mediators.
Adverse effects: Generally well-tolerated, but some patients may experience cough or throat irritation.
III. Mucolytics and Expectorants: Managing Mucus
These medications help to loosen and thin mucus, making it easier to cough up.
A. Mucolytics: Breaking Down Mucus
Mucolytics, such as acetylcysteine (N-acetylcysteine), break down the disulfide bonds in mucus, making it less viscous and easier to expectorate.
Mechanism of action: Acetylcysteine directly breaks down mucus glycoproteins.
Adverse effects: Nausea, vomiting, stomatitis (mouth sores).
B. Expectorants: Increasing Mucus Clearance
Expectorants, such as guaifenesin, increase the fluid content of mucus, making it less viscous and easier to cough up. The mechanism of action is not completely understood, but it is thought to stimulate mucus secretion and ciliary activity.
Adverse effects: Generally well-tolerated, but some patients may experience nausea or vomiting.
IV. Cough Suppressants: Controlling Cough
Cough suppressants, also known as antitussives, reduce the frequency of cough. The most common cough suppressant is codeine, a opioid. However, due to its addictive potential, it is often replaced by non-opioid alternatives such as dextromethorphan.
Mechanism of action: Codeine acts centrally on the cough center in the brain. Dextromethorphan's mechanism is less clear but it is also considered a centrally acting antitussive.
Adverse effects: Codeine can cause constipation, drowsiness, and respiratory depression. Dextromethorphan can cause drowsiness, dizziness, and nausea.
V. Drugs Affecting Respiratory Function: Potential for Harm
Several classes of drugs can negatively impact respiratory function, either directly or indirectly:
A. Opioids: Respiratory Depression
Opioids, such as morphine and codeine, are potent respiratory depressants. They act on opioid receptors in the brainstem, suppressing respiratory drive. This effect can be particularly dangerous in patients with underlying respiratory disease.
Adverse effects: Respiratory depression, drowsiness, constipation, nausea, vomiting.
B. Sedatives and Hypnotics: CNS Depression
Sedatives and hypnotics, such as benzodiazepines and barbiturates, can depress the central nervous system (CNS), including the respiratory center. This can lead to reduced respiratory rate and depth.
Adverse effects: Drowsiness, dizziness, confusion, respiratory depression.
C. Neuromuscular Blocking Agents: Muscle Paralysis
Neuromuscular blocking agents, used during anesthesia and surgery, cause paralysis of respiratory muscles, requiring mechanical ventilation.
Adverse effects: Respiratory paralysis, muscle weakness.
VI. Drug Interactions: A Critical Consideration
Drug interactions can significantly impact the efficacy and safety of respiratory medications. For example, some drugs may enhance or inhibit the metabolism of respiratory medications, altering their plasma concentrations. Other drugs may have additive respiratory depressant effects. Always consult a healthcare professional or pharmacist to assess potential drug interactions.
VII. Patient Education: A Crucial Component
Effective management of respiratory diseases requires a multi-faceted approach, including patient education. Patients should be thoroughly educated about their medications, including their purpose, dosage, administration, potential side effects, and how to manage adverse events. This collaboration empowers patients to take an active role in managing their respiratory health.
VIII. Conclusion
The management of respiratory diseases involves a range of medications with distinct mechanisms of action and potential side effects. Understanding the pharmacodynamics and pharmacokinetics of these drugs is crucial for effective and safe treatment. This knowledge base, combined with patient education and careful monitoring, contributes significantly to improving patient outcomes and quality of life. Remember, this information is for educational purposes only and should not be interpreted as medical advice. Always consult with a healthcare professional for any concerns related to your respiratory health or medication regimen.
Latest Posts
Latest Posts
-
Load Chart Values Can Pinpoint Failures Of
Apr 02, 2025
-
What Must You Do If You Suspect Iphone Efb Tampering
Apr 02, 2025
-
How Was Most Solid Waste Handled In The Middle Ages
Apr 02, 2025
-
Jonas Is A Whole Life Insurance Policyowner
Apr 02, 2025
-
The Number Of Subordinates That One Supervisor Can Manage Effectively
Apr 02, 2025
Related Post
Thank you for visiting our website which covers about Drugs Affecting The Respiratory System Edapt Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
