Esophageal Varices Most Commonly Occur In Patients Who Quizlet
Breaking News Today
Mar 18, 2025 · 6 min read
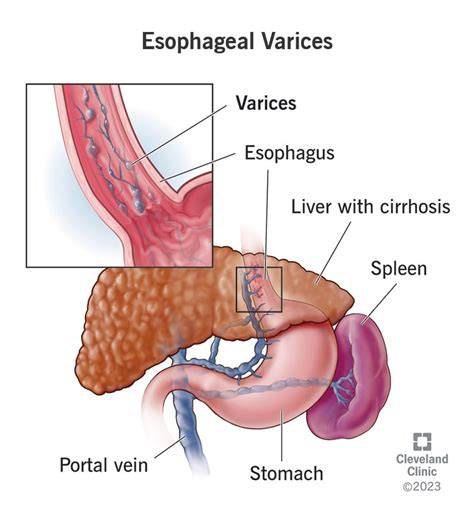
Table of Contents
Esophageal Varices: Most Commonly Occur in Patients Who...
Esophageal varices are abnormally enlarged veins in the lower part of the esophagus. These varices are a serious complication, most often stemming from portal hypertension. Understanding who is most at risk for developing esophageal varices is crucial for preventative measures and timely intervention. This comprehensive article explores the patient demographics, underlying conditions, and risk factors significantly associated with the development of esophageal varices.
Understanding Portal Hypertension: The Root Cause
Before delving into the patient populations most affected, it's essential to grasp the underlying mechanism: portal hypertension. This condition involves an increase in blood pressure within the portal venous system, which carries blood from the digestive organs to the liver. The liver is vital in processing nutrients and filtering toxins from this blood. When the liver's function is compromised, or the flow of blood through the liver is obstructed, pressure builds up in the portal vein.
This increased pressure forces blood to seek alternative pathways, leading to the dilation of veins in the esophagus (esophageal varices), stomach (gastric varices), and rectum (rectal varices). These dilated veins are fragile and prone to rupture, causing life-threatening bleeding.
Key Factors Leading to Portal Hypertension
Several factors contribute to portal hypertension. The most common include:
- Cirrhosis: This is the most significant cause. Cirrhosis, a late stage of scarring (fibrosis) of the liver, disrupts the liver's architecture and impedes blood flow. The scarring is often a consequence of chronic liver diseases.
- Hepatitis B and C: These viral infections are major culprits in causing chronic liver disease, leading to cirrhosis and, subsequently, portal hypertension.
- Alcohol Abuse: Chronic alcohol consumption is a leading cause of cirrhosis and liver damage, substantially increasing the risk of esophageal varices.
- Non-alcoholic Fatty Liver Disease (NAFLD): The prevalence of NAFLD is rising globally, primarily linked to obesity, diabetes, and metabolic syndrome. NAFLD can progress to cirrhosis and portal hypertension.
- Schistosomiasis: This parasitic infection can cause significant liver damage and fibrosis, leading to portal hypertension.
- Hepatic Vein Thrombosis (Budd-Chiari Syndrome): This rare condition involves blood clots blocking the hepatic veins, which drain blood from the liver. The resulting back-up of blood causes portal hypertension.
- Congenital Abnormalities: In rare cases, structural abnormalities in the portal venous system can contribute to portal hypertension.
Patient Populations Most at Risk: A Detailed Look
Based on the underlying causes, several patient populations are identified as having a significantly higher risk of developing esophageal varices:
1. Patients with Cirrhosis: The Largest Group
Cirrhosis of any etiology stands as the primary risk factor. This encompasses cirrhosis resulting from alcohol abuse, viral hepatitis, NAFLD, autoimmune liver diseases, and other chronic liver conditions. The severity of cirrhosis strongly correlates with the risk of developing esophageal varices. Patients with advanced cirrhosis (Child-Pugh class C) are at the highest risk.
Keywords: cirrhosis, liver cirrhosis, end-stage liver disease, alcoholic cirrhosis, viral hepatitis cirrhosis, NAFLD cirrhosis, Child-Pugh class C, liver failure
2. Patients with Chronic Hepatitis B and C Infections: A Persistent Threat
Untreated or poorly managed chronic hepatitis B and C infections are major drivers of liver damage and cirrhosis. The persistent inflammation and eventual fibrosis caused by these viruses place individuals at a high risk of developing esophageal varices over time.
Keywords: hepatitis B, hepatitis C, chronic hepatitis, viral hepatitis, liver inflammation, liver fibrosis, antiviral treatment
3. Patients with Alcohol-Related Liver Disease: A Preventable Risk
Long-term, heavy alcohol consumption is a significant risk factor. Alcohol directly damages liver cells, initiating a cascade of events that can culminate in cirrhosis and portal hypertension. The longer and heavier the alcohol consumption, the greater the risk.
Keywords: alcohol abuse, alcohol-related liver disease, alcoholic hepatitis, alcoholic cirrhosis, alcohol withdrawal, liver damage
4. Patients with Non-alcoholic Fatty Liver Disease (NAFLD): A Growing Concern
NAFLD is rapidly becoming a leading cause of chronic liver disease worldwide. Obesity, type 2 diabetes, and metabolic syndrome are strong contributors. The accumulation of fat in the liver leads to inflammation, fibrosis, and eventually cirrhosis, substantially increasing the risk of esophageal varices.
Keywords: non-alcoholic fatty liver disease, NAFLD, NASH, obesity, type 2 diabetes, metabolic syndrome, insulin resistance, fatty liver
5. Patients with Schistosomiasis: A Neglected Tropical Disease
Schistosomiasis, a parasitic infection prevalent in certain parts of the world, can cause significant liver damage and fibrosis, leading to portal hypertension and esophageal varices. This highlights the importance of public health initiatives aimed at preventing and treating schistosomiasis.
Keywords: schistosomiasis, parasitic infection, liver fluke, portal hypertension, neglected tropical diseases, public health
6. Patients with Budd-Chiari Syndrome: A Rare but Serious Cause
Budd-Chiari syndrome, a rare condition causing blockage of the hepatic veins, creates significant back-pressure in the portal venous system. This directly leads to portal hypertension and a heightened risk of esophageal varices.
Keywords: Budd-Chiari syndrome, hepatic vein thrombosis, hepatic vein occlusion, portal vein hypertension, rare liver disease
7. Patients with Other Liver Diseases: A Broader Perspective
Beyond the conditions mentioned above, other liver diseases can contribute to portal hypertension and esophageal varices. These include autoimmune liver diseases like autoimmune hepatitis, primary biliary cholangitis, and primary sclerosing cholangitis. Genetic disorders affecting liver function can also increase the risk.
Recognizing the Symptoms: Early Detection is Key
Recognizing the symptoms of esophageal varices, particularly bleeding, is critical for timely intervention. While often asymptomatic until rupture, signs can include:
- Upper gastrointestinal bleeding: This is the most serious manifestation, presenting as hematemesis (vomiting blood) or melena (black, tarry stools).
- Abdominal pain: Pain may be present, particularly if there's bleeding or inflammation.
- Weakness and dizziness: Significant blood loss can lead to these symptoms.
Management and Prevention: A Multifaceted Approach
Management of esophageal varices focuses on preventing bleeding and treating complications. This typically involves:
- Beta-blockers: These medications help reduce portal pressure.
- Endoscopic therapies: Procedures like banding or sclerotherapy can eliminate varices.
- Transjugular intrahepatic portosystemic shunt (TIPS): A surgical procedure that creates a shunt to divert blood flow, reducing portal pressure.
- Liver transplant: In severe cases, a liver transplant may be necessary.
Prevention centers around managing the underlying liver disease, avoiding alcohol, maintaining a healthy weight, and adhering to prescribed medication.
Conclusion: A Call to Awareness and Action
Esophageal varices are a serious complication of portal hypertension, most commonly associated with cirrhosis of various etiologies. Understanding the patient populations at greatest risk – those with cirrhosis, chronic viral hepatitis, alcohol-related liver disease, NAFLD, schistosomiasis, and Budd-Chiari syndrome – is vital for proactive screening, early diagnosis, and prompt management. Early detection and appropriate medical intervention are crucial to minimizing the risk of life-threatening complications. Public health initiatives aimed at preventing chronic liver disease and managing underlying risk factors play a crucial role in reducing the incidence of esophageal varices and improving patient outcomes. This multifaceted approach, combining awareness, prevention, and effective management strategies, is essential to addressing this significant health concern.
Latest Posts
Latest Posts
-
Kaz Wants To Stop Biting His Nails
Mar 21, 2025
-
Letrs Unit 4 Session 8 Check For Understanding
Mar 21, 2025
-
Which Of The Following Is Most Associated With Managerial Accounting
Mar 21, 2025
-
The Planning Steps Of The Planning Control Cycle Are
Mar 21, 2025
-
The Nose Is Located Blank And Blank To The Ears
Mar 21, 2025
Related Post
Thank you for visiting our website which covers about Esophageal Varices Most Commonly Occur In Patients Who Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
