If A Resident Is In Shock A Nursing Assistant Should
Breaking News Today
Mar 17, 2025 · 7 min read
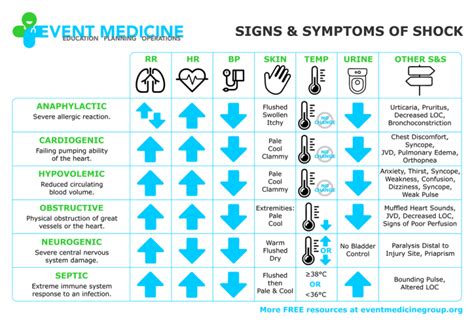
Table of Contents
If a Resident is in Shock: A Nursing Assistant's Crucial Role
Shock is a life-threatening condition characterized by inadequate blood flow to the body's organs and tissues. As a nursing assistant, recognizing the signs and symptoms of shock and knowing how to respond effectively is crucial for ensuring the resident's safety and survival. This article will detail the essential steps a nursing assistant should take if they encounter a resident in shock, emphasizing prompt action and effective communication. We will cover recognizing the signs, initiating immediate actions, and collaborating with the nursing team for comprehensive care.
Recognizing the Signs of Shock: Early Detection is Key
Early recognition of shock is paramount. The symptoms can vary depending on the underlying cause, but some common indicators include:
Vital Sign Changes:
- Hypotension (Low Blood Pressure): This is a key sign, indicating the body's inability to maintain adequate blood flow. Note that hypotension is not always present in early stages, especially in elderly individuals.
- Tachycardia (Rapid Heart Rate): The heart attempts to compensate for low blood volume by beating faster.
- Tachypnea (Rapid Breathing): The body tries to increase oxygen intake.
- Weak or Absent Peripheral Pulses: Reduced blood flow to the extremities.
- Cool, Clammy Skin: Due to peripheral vasoconstriction (narrowing of blood vessels).
Other Manifestations:
- Altered Mental Status: Confusion, restlessness, anxiety, or lethargy. This can range from mild disorientation to unconsciousness.
- Pale or Ashen Skin: Lack of blood flow results in a pale complexion. This is particularly noticeable in light-skinned individuals. In darker-skinned individuals, look for pallor in the mucous membranes (lips, gums).
- Excessive Thirst: The body attempts to compensate for fluid loss.
- Nausea and Vomiting: Often associated with decreased blood flow to the gastrointestinal system.
- Weakness and Dizziness: Due to insufficient oxygen reaching the brain and other organs.
Immediate Actions: Prioritizing Resident Safety
If you suspect a resident is in shock, immediate action is critical. Follow these steps while simultaneously calling for immediate medical assistance:
1. Assess the Scene and Ensure Safety:
Before approaching the resident, quickly assess the environment for any immediate dangers. This could include hazards that may have contributed to the shock (e.g., a fall, a medication error) or risks that could further endanger the resident. Make the area safe for both yourself and the resident.
2. Check the Resident's ABCs:
- Airway: Ensure the resident's airway is open and clear. If necessary, gently reposition their head to maintain an open airway.
- Breathing: Assess their breathing rate and depth. Is it rapid, shallow, or labored? If the resident is not breathing, initiate CPR as per your training.
- Circulation: Check for a pulse (carotid or femoral). Assess the skin for color, temperature, and moisture. Note the presence and strength of peripheral pulses.
3. Position the Resident:
Generally, place the resident in a supine position (lying flat on their back) with their legs elevated about 12 inches. This helps increase blood flow to vital organs. However, this positioning is contraindicated in certain types of shock, such as cardiogenic shock. If the resident has any difficulty breathing in this position, place them in a semi-Fowler's position (slightly elevated). Always prioritize maintaining a clear airway.
4. Maintain Body Temperature:
Shock can lead to hypothermia (low body temperature). Use blankets to keep the resident warm. Avoid excessive warmth, as this can worsen the condition.
5. Monitor Vital Signs:
Continuously monitor the resident's vital signs (heart rate, respiratory rate, blood pressure, oxygen saturation if available) and document your findings accurately. Report any changes immediately to the nurse.
6. Provide Comfort and Reassurance:
The resident may be experiencing fear and anxiety. Offer words of comfort and reassurance, speaking in a calm and soothing voice. Maintain a calm demeanor yourself; your composure can be reassuring to the resident.
7. Prevent Further Complications:
- Avoid unnecessary movements: Minimize handling to prevent further stress on the circulatory system.
- Do not give the resident anything to eat or drink: This may interfere with medical treatment.
- Do not attempt to treat the underlying cause of shock: This is the responsibility of the medical team. Your focus is on providing basic supportive care.
Collaboration with the Nursing Team: A Unified Approach
As a nursing assistant, your role is crucial in the initial response to shock. However, you are part of a larger healthcare team. Effective communication and collaboration are vital.
8. Immediately Notify the Nurse:
Clearly and concisely report your observations and actions to the nurse. Provide detailed information about the resident's condition, including vital signs, symptoms, and any potential causes.
9. Assist with Medical Interventions:
The nurse may request your assistance with various medical interventions, such as applying oxygen, obtaining a blood sample, or preparing the resident for transport to the hospital. Follow their instructions carefully and accurately.
10. Document Thoroughly:
Accurate and complete documentation is essential. Record the time you observed the signs of shock, the actions you took, the resident's response, and any changes in their condition. This information is vital for the medical team to understand the course of events and develop an effective treatment plan. This includes noting the time of any interventions and the response.
Types of Shock and Considerations: A Deeper Dive
Different types of shock necessitate slightly different approaches, though the basic principles of maintaining airway, breathing, and circulation remain the same. Knowing these distinctions can help you better understand the situation and communicate effectively with the nursing staff.
Hypovolemic Shock: Caused by significant blood or fluid loss (e.g., hemorrhage, severe dehydration). The key is to control the source of bleeding (if present) and administer intravenous fluids (by the nurse).
Cardiogenic Shock: Occurs when the heart fails to pump enough blood to meet the body's needs. The resident may be experiencing chest pain or shortness of breath. Positioning with legs elevated may be harmful in this instance; support the resident in a semi-Fowler's position or other position determined by the nurse. Oxygen supplementation is crucial.
Septic Shock: A severe response to an infection. The resident may exhibit high fever, rapid breathing, and altered mental status. Antibiotics will be required.
Anaphylactic Shock: A severe allergic reaction. Epinephrine is the immediate treatment of choice. Early recognition and administration of epinephrine are life-saving.
Neurogenic Shock: Caused by damage to the nervous system, often from spinal cord injury. The resident may present with hypotension and bradycardia (slow heart rate). Careful management of blood pressure is necessary.
Note: This is not an exhaustive list, and the presentation of shock can be highly variable. As a nursing assistant, your role is to recognize signs and symptoms that indicate a potential emergency, act promptly, and alert the appropriate medical personnel. Do not attempt to diagnose or treat the resident independently; your primary focus should be on providing basic life support and communicating effectively with the nursing staff.
Ongoing Monitoring and Post-Shock Care: A Holistic Approach
Even after initial stabilization, ongoing monitoring is crucial. The resident may require ongoing care and support to prevent complications. Your role involves:
- Continuous Monitoring of Vital Signs: Regularly check the resident's vital signs and report any significant changes.
- Monitoring for any Changes in Condition: Observe the resident for signs of deterioration or improvement.
- Assistance with Mobility and Activities of Daily Living: The resident may require assistance with basic tasks such as eating, drinking, and toileting.
- Emotional Support: Provide comfort and reassurance to the resident and their family.
Conclusion: Empowering Nursing Assistants in Critical Situations
Shock is a medical emergency demanding swift and accurate responses. Nursing assistants play a crucial role in recognizing the signs of shock, initiating immediate life-saving measures, and collaborating effectively with the nursing team. By mastering the skills and knowledge outlined in this article, you are empowered to make a significant difference in the lives of your residents, potentially saving lives through prompt action and effective communication. Remember, ongoing education and training are essential for maintaining your competency in managing such critical situations. Your vigilance and preparedness are invaluable assets in providing high-quality resident care.
Latest Posts
Latest Posts
-
Which Best Describes The Terrorist Planning Cycle
Mar 18, 2025
-
Cdl Combination Test Questions And Answers Pdf
Mar 18, 2025
-
Life Insurance Exam Questions And Answers Pdf
Mar 18, 2025
-
The Direct Carry Is Used To Transfer A Patient
Mar 18, 2025
-
The Emancipation Proclamation Of January 1 1863 Quizlet
Mar 18, 2025
Related Post
Thank you for visiting our website which covers about If A Resident Is In Shock A Nursing Assistant Should . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
