What Action Is Not Part Of The Acute Stroke Pathway
Breaking News Today
Mar 28, 2025 · 5 min read
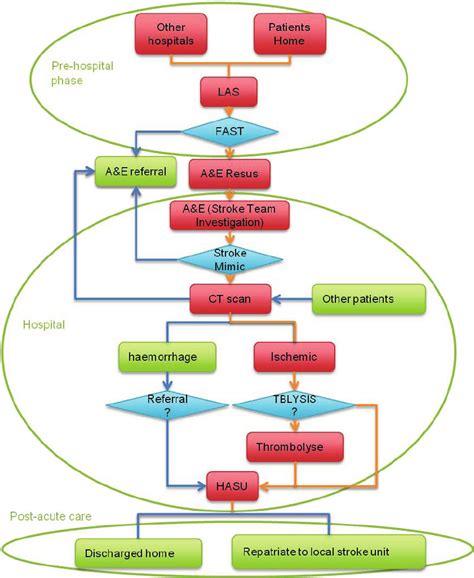
Table of Contents
What Actions Are NOT Part of the Acute Stroke Pathway? A Comprehensive Guide
A stroke, a sudden interruption of blood flow to the brain, is a time-critical medical emergency. The faster a patient receives treatment, the better their chances of recovery. This is why the acute stroke pathway exists – a streamlined process designed to rapidly diagnose and treat stroke patients. However, delays or incorrect actions can significantly hinder this process and worsen outcomes. Understanding what isn't part of the acute stroke pathway is just as crucial as knowing what is. This comprehensive guide clarifies actions that should be avoided to ensure efficient and effective stroke care.
Delays in Seeking Medical Attention: The Biggest Culprit
Perhaps the most detrimental action outside the acute stroke pathway is delaying a call for emergency medical services (EMS). Recognizing the signs of a stroke – sudden numbness or weakness in the face, arm, or leg; confusion; trouble speaking or understanding; trouble seeing; trouble walking; dizziness; severe headache – is the first step. But hesitation to call for help can be catastrophic. Every minute counts, as brain cells are dying.
Common Reasons for Delay:
- Minimizing symptoms: Many individuals attribute stroke symptoms to other, less serious conditions like fatigue or stress. This delay can lead to irreversible brain damage.
- Fear of hospitals or medical procedures: Anxiety surrounding hospitalization or medical interventions can prevent prompt action.
- Unfamiliarity with stroke symptoms: Lack of awareness regarding stroke signs can lead to delayed recognition and delayed call for help. Education is key in combating this.
- Reluctance to bother emergency services: Some individuals hesitate to call EMS, fearing it might be an unnecessary inconvenience. This is a critical misconception—prompt medical attention is always preferable in suspected stroke cases.
Inappropriate Pre-Hospital Actions: What NOT to Do
Before EMS arrives, well-intentioned but misguided actions can inadvertently harm the patient. These actions should be strictly avoided:
1. Administering Medications Without Medical Supervision:
Giving any medication, including over-the-counter drugs or home remedies, without explicit medical instruction is strictly prohibited. This includes aspirin, which, while sometimes beneficial in stroke treatment, should only be administered under the guidance of medical professionals. Improper medication can worsen the condition or interfere with diagnostic testing.
2. Attempting to "Wake Up" the Patient:
If the patient is unresponsive, resist the urge to shake or forcefully rouse them. This can cause further injury. Simply monitor their breathing and await the arrival of medical professionals.
3. Providing Food or Drink:
The patient might have difficulty swallowing (dysphagia), a common complication of stroke. Providing food or drink could lead to choking and aspiration pneumonia, posing a serious threat. Keep the patient NPO (nothing by mouth) until a medical professional assesses their condition.
4. Moving the Patient Unless Absolutely Necessary:
Unless the patient is in immediate danger (like a fire), avoid moving them. Moving could worsen the injury and complicate assessment and treatment. If the patient needs to be moved, it should only be done by trained medical personnel, using proper techniques to minimize further harm.
Inefficient Actions in the Hospital Setting:
Once the patient reaches the hospital, the clock continues to tick. Delays within the hospital system are equally detrimental. The following actions should be avoided:
1. Delays in Neuroimaging:
Prompt CT or MRI scanning is vital for diagnosing the type of stroke (ischemic or hemorrhagic) and guiding treatment decisions. Any delay in obtaining these scans can significantly impact the effectiveness of treatment. This necessitates clear communication and coordination between emergency medical services, the emergency department, and the neurology team.
2. Failure to Administer Thrombolytic Therapy (tPA) in a Timely Manner:
For ischemic stroke (caused by a blood clot), intravenous tissue plasminogen activator (tPA) is a crucial time-sensitive treatment. This clot-busting drug must be administered within a specific time window (usually 4.5 hours from symptom onset, potentially extended under certain circumstances with advanced imaging). Delays in administering tPA can drastically reduce its effectiveness and limit the chances of a positive outcome.
3. Inadequate Monitoring of Vital Signs:
Continuous and meticulous monitoring of vital signs (blood pressure, heart rate, respiratory rate, oxygen saturation, temperature) is paramount. Fluctuations in these parameters can indicate complications or worsening condition. Inadequate monitoring can lead to missed opportunities for timely intervention.
4. Insufficient Communication and Coordination Among Healthcare Professionals:
Effective communication and seamless coordination between various medical personnel—emergency medical technicians, emergency department physicians, neurologists, radiologists, nurses, and other specialists—are essential. Breakdown in communication can lead to delays, errors, and compromised patient care. This includes clear and concise documentation of every step of the process.
5. Neglecting to Address Secondary Stroke Prevention:
After the acute phase, addressing secondary stroke prevention is critical. This includes lifestyle modifications (diet, exercise, smoking cessation), medication management (blood thinners, blood pressure control), and regular follow-up appointments. Failing to prioritize these steps increases the risk of future strokes.
Lack of Patient and Family Education: A Critical Omission
The acute stroke pathway is not only about the medical interventions but also about ensuring the patient and their family understand the process and their role. Lack of education leads to anxiety, misunderstanding, and poor adherence to treatment plans.
Key Educational Components:
- Recognizing stroke symptoms: Equipping patients and their families with the knowledge to identify stroke signs promptly is paramount.
- Understanding the importance of time: Emphasizing the time-sensitive nature of stroke treatment can encourage quicker responses.
- Knowing the treatment options: Explaining the different treatment modalities (tPA, endovascular therapy, supportive care) and their implications aids informed decision-making.
- Post-stroke rehabilitation: Providing information about rehabilitation services and their importance in recovery ensures that patients are well-prepared for the long road ahead.
Conclusion: Every Second Matters
The acute stroke pathway is a meticulously designed process aiming to optimize stroke care. Understanding the actions that aren't part of this pathway—delays in seeking help, inappropriate pre-hospital interventions, inefficiencies in the hospital setting, and a lack of patient education—is crucial for improving outcomes. By avoiding these pitfalls and emphasizing proactive measures, we can significantly enhance the chances of successful recovery for stroke patients. Remember, in stroke care, every second matters. The faster and more efficiently the pathway is followed, the greater the potential for positive outcomes and improved quality of life for survivors.
Latest Posts
Latest Posts
-
Comedy Is To Laughter As Insecurity Is To
Mar 30, 2025
-
Which Of The Following Poses A Physical Security Risk
Mar 30, 2025
-
Which One Of These Is An Amino Group
Mar 30, 2025
-
Which Of The Following Statements Is True About Managerial Compensation
Mar 30, 2025
-
Ordered A Blockade To Prevent Trade And Communication
Mar 30, 2025
Related Post
Thank you for visiting our website which covers about What Action Is Not Part Of The Acute Stroke Pathway . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
