Which Event Must Precede All Others During Tissue Repair
Breaking News Today
Mar 25, 2025 · 5 min read
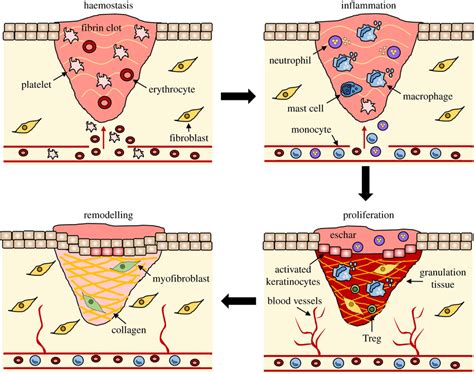
Table of Contents
Which Event Must Precede All Others During Tissue Repair?
The intricate process of tissue repair is a marvel of biological engineering, a finely orchestrated symphony of cellular and molecular events designed to restore damaged tissues to their functional state. While the entire process is a complex interplay of multiple phases, one event stands out as the absolute prerequisite for all others: hemostasis. Without the successful completion of hemostasis, the subsequent stages of inflammation, proliferation, and remodeling cannot proceed effectively, and the repair process risks failure, leading to complications such as excessive bleeding, infection, and impaired wound healing.
The Crucial Role of Hemostasis in Tissue Repair
Hemostasis, the process of stopping bleeding, is the foundational step in tissue repair. It involves a tightly regulated cascade of events aimed at preventing further blood loss and creating a stable environment conducive to the subsequent repair phases. This critical first step sets the stage for all subsequent cellular and molecular interactions. Failure at this stage can lead to significant complications, including:
- Excessive blood loss: Obvious and potentially life-threatening, uncontrolled bleeding deprives the surrounding tissues of oxygen and nutrients, hindering their ability to heal.
- Formation of hematoma: A large blood clot can physically interfere with tissue regeneration, creating a space-occupying lesion that impedes the process of cellular migration and tissue remodeling.
- Increased risk of infection: Blood provides an ideal culture medium for bacteria. Failure to control bleeding leaves the wound vulnerable to infection, potentially delaying healing and leading to serious complications.
The Stages of Hemostasis: A Coordinated Response
Hemostasis is not a single event but rather a coordinated sequence of three major stages:
1. Vascular Spasm: The immediate response to injury involves vasoconstriction, a narrowing of the blood vessels at the injury site. This reduces blood flow to the area, minimizing blood loss while the other hemostatic mechanisms are activated. This initial vasoconstriction is mediated by neurogenic reflexes and the release of vasoactive substances from platelets and the damaged endothelium.
2. Platelet Plug Formation: Platelets, small cell fragments circulating in the blood, play a crucial role in forming a temporary plug that seals the injured vessel. Upon contact with the exposed collagen fibers in the damaged tissue, platelets undergo activation, changing their shape and becoming sticky. This allows them to adhere to the collagen and to each other, forming a platelet plug that initially arrests bleeding. The release of factors like adenosine diphosphate (ADP) and thromboxane A2 further amplifies platelet aggregation.
3. Coagulation Cascade: This is the most complex phase of hemostasis, involving a cascade of enzymatic reactions that ultimately result in the formation of a stable fibrin clot. The coagulation cascade can be broadly divided into the intrinsic, extrinsic, and common pathways. The intrinsic pathway is activated by contact with negatively charged surfaces exposed by the injured vessel, while the extrinsic pathway is triggered by the release of tissue factor from damaged cells. Both pathways converge on the common pathway, culminating in the activation of thrombin, which converts soluble fibrinogen into insoluble fibrin. Fibrin forms a mesh-like structure that strengthens the platelet plug, forming a stable clot that effectively seals the damaged vessel.
The Importance of Fibrinolysis: While clot formation is crucial to stop bleeding, the fibrin clot needs to be eventually removed to allow for tissue regeneration and prevent excessive scar formation. Fibrinolysis, the breakdown of the fibrin clot, is a tightly regulated process mediated by plasmin, an enzyme that dissolves the fibrin mesh. This carefully controlled process ensures that the clot is removed only when it has served its purpose.
The Interdependence of Hemostasis and Subsequent Repair Stages
The successful completion of hemostasis is not merely a prerequisite; it fundamentally influences the subsequent stages of tissue repair. A poorly controlled or incomplete hemostatic response can have far-reaching consequences:
-
Inflammation: An adequate hemostatic response is essential for controlling the inflammatory response. The inflammatory cells recruited to the site of injury must navigate through a stable extracellular matrix, a condition best achieved when hemostasis is complete. Uncontrolled bleeding can interfere with the recruitment and function of these cells, delaying or impairing the inflammatory phase.
-
Proliferation: The proliferation phase involves the growth of new blood vessels (angiogenesis) and the synthesis of new extracellular matrix by fibroblasts. This process requires a stable environment, which hemostasis provides. The presence of blood or a hematoma can disrupt cell migration and inhibit the formation of new tissue.
-
Remodeling: The final phase of tissue repair involves the reorganization of the newly formed tissue and the maturation of the scar. The presence of blood clots or inflammation can interfere with the proper alignment of collagen fibers and the overall structural integrity of the repaired tissue. This can result in weaker scars and a higher risk of complications.
Clinical Implications of Hemostatic Failure in Tissue Repair
Failures in hemostasis can lead to various clinical complications, including:
-
Delayed Wound Healing: Poor hemostasis can prolong the healing process, increasing the risk of infection and impairing functional recovery.
-
Wound Dehiscence: This refers to the separation of the wound edges, often due to inadequate strength of the repaired tissue resulting from incomplete hemostasis.
-
Hypertrophic Scars and Keloids: Excessive or prolonged inflammation can lead to the formation of hypertrophic scars or keloids, which are raised, thickened scars that can cause pain and cosmetic problems.
-
Infection: Failure to control bleeding leaves the wound susceptible to bacterial infection, leading to further complications and potentially serious illness.
Conclusion: Hemostasis – The Foundation of Tissue Repair
In the intricate and multifaceted process of tissue repair, hemostasis undeniably holds the primary position. It's not simply a step in the sequence; it's the essential foundation upon which all other events depend. Without the efficient and complete cessation of bleeding, the inflammatory response is compromised, the proliferation of new tissue is hindered, and the remodeling process is impaired. A thorough understanding of the mechanisms of hemostasis and its profound impact on tissue repair is crucial for clinicians and researchers alike, enabling the development of better strategies for wound management and the treatment of conditions affecting tissue regeneration. The intricate dance of cellular and molecular events in tissue repair only begins when the bleeding stops. Hemostasis is not just a step; it is the cornerstone of successful tissue repair.
Latest Posts
Latest Posts
-
The Rondo May Be Schematically Outlined As
Mar 26, 2025
-
Which Three Of The Following Statements Are True
Mar 26, 2025
-
What Is The Most Dangerous Aspect Of Synergism
Mar 26, 2025
-
Benefits Provided By A Medicare Supplement Policy Must Not
Mar 26, 2025
-
Wall Street Prep Excel Crash Course Exam Answers
Mar 26, 2025
Related Post
Thank you for visiting our website which covers about Which Event Must Precede All Others During Tissue Repair . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
