Which Statement Is True Regarding Gestational Diabetes
Breaking News Today
Mar 15, 2025 · 8 min read
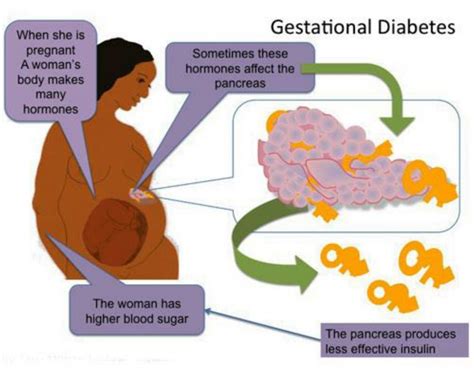
Table of Contents
Which Statement is True Regarding Gestational Diabetes? Demystifying the Facts
Gestational diabetes (GDM) is a condition affecting pregnant women characterized by high blood sugar levels. While often temporary, it presents significant implications for both mother and baby. Understanding GDM is crucial for effective management and preventing long-term health consequences. This comprehensive article will delve into various statements about GDM, separating fact from fiction and providing you with the most accurate and up-to-date information.
Understanding Gestational Diabetes: Separating Fact from Fiction
Before we delve into specific statements, let's lay a strong foundation. GDM develops during pregnancy, typically diagnosed between 24 and 28 weeks. While the exact cause remains unclear, factors like genetics, obesity, and ethnicity play a significant role. The body's inability to produce sufficient insulin or utilize it effectively leads to elevated blood glucose. This imbalance can have far-reaching consequences if left unmanaged.
Many misconceptions surround GDM. Let's address some common statements and determine their veracity:
Statement 1: "Gestational diabetes only affects women who are overweight or obese."
FALSE. While obesity significantly increases the risk of developing GDM, it's not the sole determinant. Women of normal weight can also develop this condition. Genetic predisposition, family history of diabetes, and ethnicity are all contributing factors. Women with a previous history of GDM are also at a significantly higher risk during subsequent pregnancies. Therefore, a healthy lifestyle doesn't guarantee immunity from GDM; regular screening remains crucial for all pregnant women.
Statement 2: "Gestational diabetes always disappears after delivery."
PARTIALLY TRUE. In most cases, blood sugar levels return to normal after childbirth. However, this doesn't negate the importance of careful post-partum monitoring. Women with GDM have a significantly increased risk of developing type 2 diabetes later in life. The pregnancy itself can accelerate the onset of insulin resistance, making future diabetes more likely. Post-partum follow-up screenings are essential to assess long-term risks and implement preventive measures.
Statement 3: "Gestational diabetes has no impact on the baby."
FALSE. GDM poses several potential risks to the developing fetus. High blood sugar levels can lead to macrosomia (excessively large baby), increasing the risk of birth complications such as shoulder dystocia during delivery. The baby may also experience hypoglycemia (low blood sugar) shortly after birth, requiring close monitoring and potential treatment. Furthermore, GDM can increase the risk of the baby developing obesity and type 2 diabetes later in life. These long-term implications underscore the importance of managing GDM effectively during pregnancy.
Statement 4: "Dietary changes alone are sufficient to manage gestational diabetes."
PARTIALLY TRUE. Dietary modifications are a cornerstone of GDM management. A balanced diet low in carbohydrates and high in fiber is crucial. Regular meal timing and portion control also play a vital role in maintaining stable blood sugar levels. However, for many women, diet alone is insufficient. Many require medication, such as insulin, to effectively control blood sugar levels and minimize risks to both mother and baby. The treatment plan is individualized and should be guided by a healthcare professional.
Statement 5: "Regular exercise is unnecessary if you have a healthy diet."
FALSE. Regular physical activity is a crucial component of GDM management. Exercise improves insulin sensitivity, making the body more efficient at utilizing glucose. Moderate-intensity exercise, such as brisk walking or swimming, for at least 30 minutes most days of the week, is recommended. Always consult with a healthcare professional before starting any new exercise routine, especially during pregnancy. Proper guidance ensures the safety and effectiveness of the exercise program.
Statement 6: "All women need a glucose tolerance test (GTT) during pregnancy."
PARTIALLY TRUE. While routine screening is recommended for all pregnant women, it's not universally mandated. Screening is typically done between 24 and 28 weeks of gestation. However, women with risk factors like obesity, family history of diabetes, or previous GDM may require earlier or more frequent testing. Individualized assessment determines the appropriate approach to screening, guided by the specific circumstances of the pregnant woman and her medical history.
Statement 7: "Having gestational diabetes increases your risk of developing other health problems."
TRUE. GDM significantly increases the risk of developing type 2 diabetes later in life. It also raises the risk of cardiovascular disease, hypertension, and polycystic ovary syndrome (PCOS). The hormonal changes and insulin resistance experienced during pregnancy can persist, predisposing women to these long-term health conditions. Therefore, maintaining a healthy lifestyle after delivery, including diet, exercise, and regular health checkups, is paramount in mitigating these future health risks.
Statement 8: "There are no long-term effects of gestational diabetes on the mother."
FALSE. As mentioned earlier, GDM can significantly increase the risk of developing type 2 diabetes, cardiovascular disease, and other health problems later in life. It’s not simply a temporary condition during pregnancy; it’s a warning sign that may indicate a predisposition to future metabolic disorders. Postnatal care and lifestyle adjustments are essential to mitigate these risks.
Statement 9: "Gestational diabetes is easily diagnosed through a simple blood test."
PARTIALLY TRUE. The diagnosis usually involves a glucose tolerance test (GTT). This involves drinking a glucose solution and having blood sugar levels measured at specific intervals. While the test is relatively simple, interpretation requires medical expertise to rule out other potential conditions. The results help determine the severity of glucose intolerance, guiding treatment decisions and management strategies.
Statement 10: "There are no effective treatments for gestational diabetes."
FALSE. Several effective treatments are available for managing GDM. These can range from dietary modifications and regular exercise to medication, primarily insulin, if necessary. The choice of treatment depends on the individual's blood glucose levels, overall health, and response to lifestyle changes. Close monitoring and regular adjustments to the treatment plan are crucial for maintaining optimal blood sugar levels throughout the pregnancy.
Comprehensive Management of Gestational Diabetes: A Multifaceted Approach
Managing GDM effectively requires a holistic approach, encompassing lifestyle adjustments and, in some cases, medication. Let's examine each facet:
Dietary Management: The Foundation of GDM Control
Nutritional therapy forms the bedrock of GDM management. It involves consuming a balanced diet with:
- Controlled Carbohydrate Intake: Focus on complex carbohydrates like whole grains, fruits, and vegetables, limiting simple sugars and refined carbohydrates.
- Increased Fiber Consumption: Fiber helps regulate blood sugar levels, promoting satiety and preventing blood glucose spikes.
- Regular Meal Timing: Eating at regular intervals helps maintain consistent blood sugar levels, avoiding drastic fluctuations.
- Portion Control: Monitoring portion sizes prevents overconsumption and subsequent blood glucose elevation.
- Lean Protein Sources: Including lean protein in meals aids in blood sugar regulation and provides essential nutrients.
- Healthy Fats: Incorporating healthy fats like avocados, nuts, and olive oil contributes to overall health and satiety.
Physical Activity: Enhancing Insulin Sensitivity
Regular physical activity plays a pivotal role in improving insulin sensitivity. Aim for at least 30 minutes of moderate-intensity exercise on most days of the week. Activities like brisk walking, swimming, or cycling are ideal. Always consult your healthcare professional before starting any new exercise routine, especially during pregnancy. The exercise plan should be tailored to your fitness level and pregnancy stage.
Medical Management: Insulin Therapy and Other Medications
In many cases, lifestyle changes alone are insufficient to control GDM. Medical intervention may be necessary, typically involving insulin therapy. Insulin injections help regulate blood sugar levels, ensuring fetal well-being. Other medications, such as metformin, may be considered in certain circumstances. The dosage and type of medication are determined on an individual basis, guided by the severity of GDM and the woman's response to treatment.
Regular Monitoring: A Crucial Element for Success
Close monitoring of blood glucose levels is essential for effective GDM management. Frequent blood sugar testing provides insights into the effectiveness of the treatment plan. Regular checkups with your healthcare provider are necessary to assess progress and make necessary adjustments. This close monitoring ensures the best possible outcome for both mother and baby.
Long-Term Implications and Preventive Measures
GDM doesn't simply disappear after childbirth. It significantly increases the risk of developing type 2 diabetes and other health problems later in life. Therefore, post-partum care and long-term lifestyle modifications are crucial. This includes maintaining a healthy diet, engaging in regular physical activity, and undergoing regular health screenings. Family history and genetics also influence the likelihood of developing future diabetes. Adopting a preventive lifestyle approach is crucial in mitigating long-term health risks.
Conclusion: Empowering Women Through Knowledge and Action
Gestational diabetes is a serious condition, but with effective management, the risks to both mother and baby can be significantly minimized. Understanding the facts, dispelling myths, and embracing a comprehensive management approach are crucial for positive outcomes. Remember, the key lies in early diagnosis, close monitoring, and a collaborative approach between the pregnant woman, her healthcare provider, and her support network. This holistic approach can help ensure a healthy pregnancy and reduce the risk of long-term complications for both mother and child. By empowering pregnant women with accurate information, we can improve their health outcomes and support their overall well-being.
Latest Posts
Latest Posts
-
What Amount Of Residual Urine Is Considered Abnormal Quizlet
Mar 18, 2025
-
Ati Rn Comprehensive Predictor 2023 With Ngn Quizlet
Mar 18, 2025
-
How Many Feet From A Helicopter Lifting Depositing Quizlet
Mar 18, 2025
-
What Is The Best Definition Of Marginal Revenue Quizlet
Mar 18, 2025
-
The Superficial Temporal Artery Can Be Palpated Quizlet
Mar 18, 2025
Related Post
Thank you for visiting our website which covers about Which Statement Is True Regarding Gestational Diabetes . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
