Which Type Of Pain Is Associated With Fibromyalgia Quizlet
Breaking News Today
Mar 18, 2025 · 6 min read
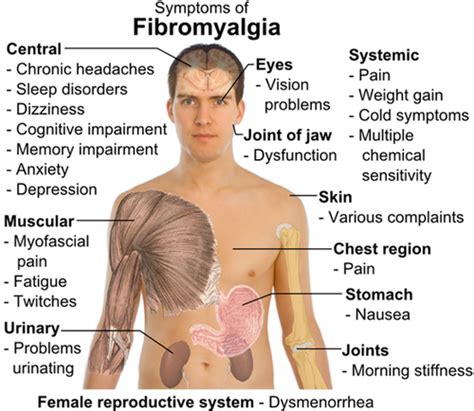
Table of Contents
Which Type of Pain is Associated with Fibromyalgia? A Comprehensive Guide
Fibromyalgia is a chronic condition characterized by widespread musculoskeletal pain accompanied by fatigue, sleep, memory, and mood issues. Understanding the specific type of pain associated with fibromyalgia is crucial for effective diagnosis and management. This article delves deep into the nature of fibromyalgia pain, exploring its characteristics, differentiating it from other pain conditions, and providing insights into its impact on daily life.
Understanding Fibromyalgia Pain: More Than Just Aches and Pains
Fibromyalgia pain isn't your typical muscle soreness after a workout. It's a complex, multifaceted experience often described as:
- Widespread: Pain is felt in both the upper and lower halves of the body, and on both sides of the body. This widespread nature is a key diagnostic criterion.
- Chronic: The pain persists for at least three months.
- Intense: The pain intensity can fluctuate, ranging from mild discomfort to debilitating agony.
- Burning/Stabbing: Many sufferers describe the pain as burning, stabbing, shooting, or aching. It’s not always localized to a specific area.
- Allodynia: This refers to pain caused by stimuli that normally wouldn't cause pain, such as light touch or pressure. Imagine the slightest touch feeling like a sharp jab.
- Hyperalgesia: This is an increased sensitivity to painful stimuli. What would normally be a mild pinch might feel intensely painful to someone with fibromyalgia.
It's important to note: Fibromyalgia pain isn't just "in the head." While psychological factors play a role in the condition's experience, the pain is very real and significantly impacts sufferers' lives.
Differentiating Fibromyalgia Pain from Other Conditions
The symptoms of fibromyalgia can overlap with numerous other conditions, making diagnosis challenging. Differentiating fibromyalgia pain requires careful consideration of several factors:
- Rheumatoid Arthritis (RA): While both involve joint pain, RA involves inflammation of the joints, leading to swelling, stiffness, and visible joint damage. Fibromyalgia, on the other hand, doesn't typically involve joint inflammation or structural damage.
- Osteoarthritis (OA): OA is characterized by cartilage breakdown in the joints, resulting in pain, stiffness, and limited range of motion. While both can involve widespread pain, OA pain is typically localized to specific joints affected by degeneration.
- Lupus: Lupus is an autoimmune disease that can cause widespread pain, fatigue, and skin rashes. However, lupus often involves other systemic symptoms, such as kidney or heart involvement, which are not typically seen in fibromyalgia.
- Chronic Fatigue Syndrome (CFS): Both fibromyalgia and CFS involve chronic fatigue, but fibromyalgia’s defining characteristic is the widespread musculoskeletal pain. CFS primarily focuses on debilitating fatigue without the prominent pain component.
- Myofascial Pain Syndrome: This condition involves pain in the muscles and fascia (connective tissue). While there's overlap in symptoms, myofascial pain syndrome usually involves more localized pain and trigger points.
The Neurological Basis of Fibromyalgia Pain
Research suggests that fibromyalgia pain originates from abnormalities in the central nervous system (CNS), specifically the brain and spinal cord. These abnormalities affect how the CNS processes pain signals.
- Central Sensitization: This is a key mechanism in fibromyalgia. It involves an increased sensitivity to pain signals, leading to amplification of even mild stimuli. The brain becomes more sensitive to pain, and even non-painful stimuli can be perceived as painful.
- Dysregulation of Neurotransmitters: Imbalances in neurotransmitters, such as serotonin and substance P, are implicated in the development and maintenance of fibromyalgia pain. These imbalances affect pain perception and processing.
- Structural Changes in the Brain: Studies have shown structural and functional changes in brain regions involved in pain processing, emotional regulation, and sleep.
The Role of Psychological Factors
While not the cause of fibromyalgia, psychological factors such as stress, anxiety, and depression can exacerbate the condition and worsen pain perception. Chronic stress can trigger central sensitization, making individuals more susceptible to experiencing pain. Furthermore, the chronic pain itself can contribute to the development of depression and anxiety, creating a vicious cycle.
Diagnosing Fibromyalgia: A Multifaceted Approach
There is no single test to diagnose fibromyalgia. Diagnosis relies on a combination of:
- Physical Examination: A doctor will assess your pain distribution, tenderness to touch (tender points), range of motion, and other physical symptoms.
- Symptom Evaluation: A thorough review of your medical history, including the duration and character of your pain, fatigue, sleep disturbances, and other symptoms.
- Exclusion of other conditions: Tests may be ordered to rule out other conditions with overlapping symptoms.
- American College of Rheumatology (ACR) criteria: While not a definitive test, these criteria provide guidelines for diagnosing fibromyalgia based on widespread pain and tender points. However, the criteria are constantly evolving, and the emphasis is shifting towards a more holistic approach, considering the broader symptom picture.
Managing Fibromyalgia Pain: A Holistic Approach
Managing fibromyalgia pain requires a multidisciplinary approach that addresses both the physical and psychological aspects of the condition. Effective management strategies include:
- Medication: Medications such as analgesics, antidepressants, and anticonvulsants can help manage pain, improve sleep, and address mood issues. The choice of medication depends on individual needs and response.
- Physical Therapy: Exercises focusing on low-impact activities, stretching, and strengthening can improve flexibility, range of motion, and reduce pain.
- Cognitive Behavioral Therapy (CBT): CBT helps individuals develop coping strategies to manage pain, stress, and improve their overall psychological well-being.
- Lifestyle Modifications: Regular exercise, stress management techniques (such as yoga or meditation), sufficient sleep, and a healthy diet can significantly impact pain levels and overall quality of life.
- Alternative Therapies: Some individuals find relief through alternative therapies such as acupuncture, massage therapy, and Tai Chi. However, it's important to discuss these options with your doctor before trying them.
The Importance of Self-Management
Self-management strategies are crucial for long-term success in managing fibromyalgia. This involves understanding your triggers, tracking your symptoms, and actively participating in your treatment plan. Developing a personalized plan that incorporates the strategies mentioned above is essential for achieving the best possible outcomes.
Living with Fibromyalgia: Challenges and Coping Mechanisms
Living with fibromyalgia can present significant challenges, affecting daily activities, work, relationships, and overall quality of life. However, with the right support and management strategies, individuals can learn to live well with the condition.
- Pain Management Strategies: Developing a personalized pain management plan that incorporates various strategies, including medication, physical therapy, and relaxation techniques, is essential.
- Emotional Support: Seeking support from family, friends, or support groups can help cope with the emotional toll of living with chronic pain.
- Adaptive Strategies: Making adjustments to daily routines and work schedules can help manage energy levels and reduce pain exacerbation.
- Self-Care: Prioritizing self-care activities, such as relaxation techniques, hobbies, and social interaction, is essential for maintaining well-being.
- Education and Advocacy: Learning about fibromyalgia and advocating for oneself in healthcare settings can empower individuals to take control of their condition.
Conclusion: A Journey Towards Better Management
Fibromyalgia pain is a complex and multifaceted experience that requires a comprehensive understanding for effective management. While a cure remains elusive, significant advancements in research and treatment have improved the lives of many sufferers. By combining medical interventions, lifestyle modifications, and psychological support, individuals can learn to manage their pain, improve their quality of life, and live fulfilling lives despite the challenges posed by this chronic condition. Remember, you are not alone, and effective management is achievable through a proactive and holistic approach. Continued research holds the promise of even better treatments and a deeper understanding of this debilitating condition in the future.
Latest Posts
Latest Posts
-
High Levels Of Cholesterol Can First Lead Directly To
Mar 18, 2025
-
True Or False Professional And Technical Communication Is Research Oriented
Mar 18, 2025
-
Which Best Describes The Terrorist Planning Cycle
Mar 18, 2025
-
Cdl Combination Test Questions And Answers Pdf
Mar 18, 2025
-
Life Insurance Exam Questions And Answers Pdf
Mar 18, 2025
Related Post
Thank you for visiting our website which covers about Which Type Of Pain Is Associated With Fibromyalgia Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
